TL;DR
Hereditary Hemorrhagic Telangiectasia (HHT) is a rare genetic disorder that causes abnormal blood vessels to form throughout the body. Key characteristics of HHT include:
- Telangiectases: Tiny, dilated blood vessels on the skin and mucous membranes.
- Arteriovenous Malformations (AVMs): Abnormal connections between arteries and veins.
- Frequent Bleeding: Nosebleeds, gastrointestinal bleeding, and pulmonary hemorrhage.
- Genetic mutations in the ENG or ALK1 genes.
- Disrupted blood vessel development and stability.
- Formation of AVMs.
- Nosebleeds
- Telangiectases
- AVMs in various organs for example in lungs (pulmonary arteriovenous malformation), brain (cerebral arteriovenous malformation) or liver
- Gastrointestinal bleeding
- Pulmonary hemorrhage
- Anemia
- Fatigue
- Shortness of breath
- Headaches
- Curaçao criteria
- Genetic testing
- Imaging tests (chest X-ray, CT scan, MRI, echocardiogram)
- Endoscopy
- Managing symptoms (nosebleeds, gastrointestinal bleeding, AVMs)
- General management (avoiding trauma, lifestyle modifications)
- Emerging therapies (gene therapy, stem cell therapy)
- Chronic anemia
- Organ damage
- Heart failure
- Stroke
- Liver dysfunction
*Click ▾ for more information
Introduction
Hereditary Hemorrhagic Telangiectasia (HHT), is a rare genetic disorder that causes abnormal blood vessels to form throughout the body. These abnormal blood vessels, called telangiectases and arteriovenous malformations (AVMs), can rupture and cause bleeding.
Key characteristics of hereditary hemorrhagic telangiectasia (HHT) include
- Telangiectases: These are tiny, dilated blood vessels that appear as red spots on the skin, mucous membranes, and internal organs. They are most commonly found on the face, lips, mouth, and fingertips.
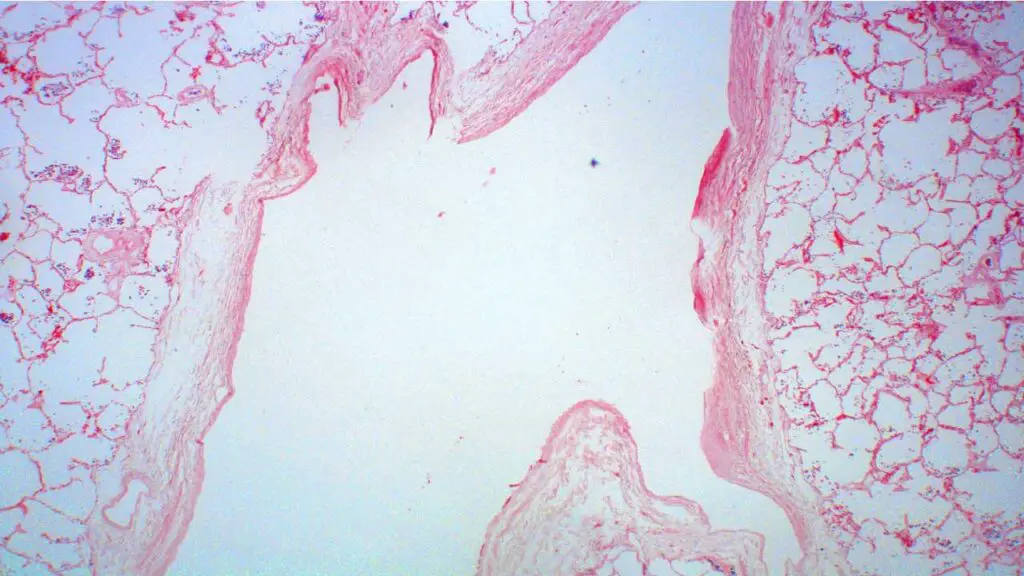
- Arteriovenous Malformations (AVMs): These are abnormal connections between arteries and veins that bypass the normal capillary network. AVMs can occur in various organs, including the lungs (pulmonary arteriovenous malformation), brain (cerebral arteriovenous malformation), liver, and gastrointestinal tract.
- Recurrent bleeding: People with hereditary hemorrhagic telangiectasia (HHT) often experience frequent nosebleeds (epistaxis), as well as bleeding from the gastrointestinal tract, lungs, and other organs.
- Inheritance: Hereditary hemorrhagic telangiectasia (HHT) is an autosomal dominant disorder, meaning that if one parent has the condition, there is a 50% chance of passing it on to their children.
It’s important to note that the severity of hereditary hemorrhagic telangiectasia (HHT) can vary greatly from person to person, even within the same family. Some individuals may experience only mild symptoms, while others may have more severe complications, such as organ failure.

Causes and Pathophysiology of Hereditary Hemorrhagic Telangiectasia (HHT)
Causes
HHT is a genetic disorder, meaning it’s inherited from a parent. It’s caused by mutations in specific genes that regulate blood vessel development. The most common genes involved are:
- Endoglin (ENG) gene: Mutations in this gene lead to HHT type 1.
- Activin receptor-like kinase 1 (ALK1) gene: Mutations in this gene lead to HHT type 2.
Pathophysiology
The exact mechanisms underlying hereditary hemorrhagic telangiectasia (HHT) are complex, but the underlying issue is a disruption in the normal development and maintenance of blood vessels. Mutations in the aforementioned genes lead to:
Defective Blood Vessel Formation
- Abnormal Signaling Pathways: The mutated genes interfere with crucial signaling pathways that regulate blood vessel growth and stability.
- Impaired Cellular Interactions: Cells involved in blood vessel development may not communicate properly, leading to abnormal vessel structures.
Weakened Blood Vessel Walls
- Reduced Structural Integrity: The blood vessel walls may be thinner and weaker than normal, making them more prone to rupture and bleeding.
- Increased Permeability: The vessel walls may allow blood cells and fluid to leak out more easily, contributing to bleeding episodes.
Formation of Arteriovenous Malformations (AVMs)
- Direct Connections: AVMs are abnormal connections between arteries and veins that bypass the capillary network.
- Increased Blood Flow: This can lead to high blood pressure and damage to the affected organs.
As a result of these underlying mechanisms, individuals with HHT experience a variety of symptoms, including:
- Telangiectases: Small, dilated blood vessels on the skin and mucous membranes.
- Recurrent Bleeding: Nosebleeds, gastrointestinal bleeding, and pulmonary hemorrhage.
- Arteriovenous Malformations: In organs like the lungs (pulmonary arteriovenous malformation), brain (cerebral arteriovenous malformation), and liver.
Symptoms of Hereditary Hemorrhagic Telangiectasia (HHT)
Hereditary Hemorrhagic Telangiectasia (HHT) is characterized by a variety of symptoms, primarily related to abnormal blood vessel formation. The most common symptoms include:
- Frequent Nosebleeds (Epistaxis): Often the earliest and most common symptom. It can range from mild to severe, sometimes occurring daily.
- Telangiectases: Small, dilated blood vessels that appear as red spots on the skin and mucous membranes. It is commonly found on the face, lips, mouth, and fingertips.
- Arteriovenous Malformations (AVMs): Abnormal connections between arteries and veins that bypass the capillary network. It can occur in various organs, including:
- Lungs (pulmonary arteriovenous malformation): May cause shortness of breath, cyanosis (bluish skin), and heart failure.
- Cerebral arteriovenous malformation: Can lead to headaches, seizures, and stroke.
- Liver: May result in liver dysfunction.
- Other potential symptoms
- Gastrointestinal bleeding: Can cause blood in the stool or anemia.
- Pulmonary hemorrhage: Coughing up blood.
- Anemia: Due to chronic blood loss.
- Fatigue: A common symptom associated with anemia and other complications.
It’s important to note that the severity of hereditary hemorrhagic telangiectasia (HHT) symptoms can vary widely among individuals. While some people may experience only mild symptoms, others may have significant health problems.
Diagnosis of Hereditary Hemorrhagic Telangiectasia (HHT)
The diagnosis of hereditary hemorrhagic telangiectasia (HHT) typically involves a combination of clinical criteria and diagnostic tests.
Clinical Criteria: Curaçao Criteria
The most commonly used diagnostic criteria for hereditary hemorrhagic telangiectasia (HHT) are the Curaçao criteria. To be diagnosed with hereditary hemorrhagic telangiectasia (HHT), a person must meet three or more of the following criteria:
- Epistaxis: Recurrent, spontaneous nosebleeds.
- Cutaneous and mucosal telangiectases: Small, dilated blood vessels on the skin and mucous membranes.
- Arteriovenous malformations (AVMs): Abnormal connections between arteries and veins in internal organs, such as the lungs (pulmonary arteriovenous malformation), brain (cerebral arteriovenous malformation), or liver.
- A first-degree relative with hereditary hemorrhagic telangiectasia (HHT): A parent, sibling, or child with a diagnosis of hereditary hemorrhagic telangiectasia (HHT).
Diagnostic Tests
To confirm the diagnosis and identify potential complications.
- Genetic testing: This test can identify specific gene mutations associated with hereditary hemorrhagic telangiectasia (HHT), such as mutations in the ENG or ALK1 genes.
- Imaging tests:
- Chest X-ray: To detect pulmonary arteriovenous malformation.
- CT scan or MRI: To assess cerebral arteriovenous malformation and liver AVM.
- Echocardiogram: To evaluate heart function and potential cardiac involvement.
- Endoscopy: To identify gastrointestinal telangiectases.
It’s important to note that early diagnosis of hereditary hemorrhagic telangiectasia (HHT) is crucial for timely management and prevention of complications.
Treatment and Management of Hereditary Hemorrhagic Telangiectasia (HHT)
While there’s currently no cure for hereditary hemorrhagic telangiectasia (HHT), various treatments can help manage symptoms and prevent complications. The specific approach to treatment will depend on the individual’s symptoms and the severity of the condition.
Managing Symptoms
- Nosebleeds
- Nasal packing: A common method to control bleeding.
- Cauterization: A technique to seal the blood vessels.
- Endoscopic procedures: To identify and treat bleeding sources.
- Medications: To help with clotting.
- Gastrointestinal bleeding
- Endoscopic procedures: To identify and treat bleeding sources.
- Medications: To reduce acid production in the stomach.
- Pulmonary arteriovenous malformation
- Interventional radiology: To block blood flow to the AVMs.
- Cerebral arteriovenous malformation
- Surgery: To remove the AVM.
- Radiosurgery: To destroy the AVM using focused radiation.
General Management
- Avoid trauma: To prevent bleeding episodes.
- Lifestyle modifications:
- Avoid aspirin and NSAIDs: These medications can increase bleeding risk.
- Maintain hydration: To prevent dehydration, especially during episodes of bleeding.
- Healthy diet: A balanced diet can help maintain overall health.
- Regular medical check-ups: To monitor for complications and adjust treatment as needed.
Complications of Hereditary Hemorrhagic Telangiectasia (HHT)
Hereditary hemorrhagic telangiectasia (HHT) can lead to a variety of complications, primarily due to bleeding and the formation of arteriovenous malformations (AVMs). Here are some of the most common complications:
Bleeding Complications
- Chronic anemia: Frequent bleeding, particularly from nosebleeds and gastrointestinal bleeding, can lead to iron deficiency anemia.
- Organ damage: Severe bleeding episodes can damage organs like the kidneys and liver.
Pulmonary Arteriovenous Malformation
- Heart strain: Increased blood flow through the lungs can put extra strain on the heart, leading to heart failure.
- Reduced oxygenation: AVMs can bypass the lungs, reducing the oxygenation of blood.
- Paradoxical embolism: Blood clots can travel from the veins to the arteries, causing strokes or other complications.
Cerebral Arteriovenous Malformation
- Stroke: Rupture of a cerebral AVM can lead to hemorrhagic stroke.
- Seizures: Abnormal electrical activity in the brain.
- Headaches: Caused by increased blood flow or pressure in the brain.
Hepatic Arteriovenous Malformation
- Liver dysfunction: Increased blood flow to the liver can lead to liver damage and cirrhosis.
- Portal hypertension: Increased pressure in the portal vein can lead to complications like esophageal varices.
Other Complications
- Iron deficiency anemia: Chronic blood loss can lead to iron deficiency.
- Fatigue: Due to anemia and other complications.
- Reduced quality of life: Frequent bleeding episodes and other symptoms can significantly impact quality of life.
It’s important to note that the severity of these complications can vary widely among individuals with HHT. Early diagnosis and appropriate management can help minimize the risk of complications and improve the overall quality of life for people with HHT.
Frequently Asked Questions (FAQs)
When do HHT symptoms start?
HHT symptoms typically start in childhood or adolescence, but can begin at any age. The most common first symptom is nosebleeds, which can start as early as infancy or as late as adulthood.
What is the life expectancy of HHT?
With appropriate treatment and regular monitoring, people with HHT can have a near-normal life expectancy. A study in 2020 found that the average life expectancy for people with HHT was 75.9 years, which is comparable to the general population. However, it’s important to note that this can vary depending on the severity of the condition and the presence of complications.
What is the most common cause of death in HHT?
The most common causes of death in HHT are:
- Cerebrovascular events: Rupture of cerebral arteriovenous malformations (AVMs) can lead to strokes.
- Pulmonary complications: Pulmonary AVMs can lead to heart failure and respiratory problems.
- Severe bleeding episodes: Severe bleeding, particularly from the gastrointestinal tract or lungs, can be life-threatening.
While HHT can significantly impact quality of life and lead to complications, with proper management and treatment, many people with HHT can live long and fulfilling lives.
What makes telangiectasia worse?
Several factors can exacerbate telangiectasia.
Environmental Factors
- Sun exposure: Prolonged sun exposure can worsen telangiectasia, especially on the face and neck.
- Extreme temperatures: Both hot and cold temperatures can aggravate the condition.
- Wind exposure: Wind can irritate the skin and worsen telangiectasia.
Lifestyle Factors
- Alcohol consumption: Excessive alcohol consumption can dilate blood vessels, worsening telangiectasia.
- Smoking: Smoking can damage blood vessels and contribute to the development of telangiectasia.
- Spicy foods: Spicy foods can cause flushing, which can temporarily worsen the appearance of telangiectasia.
Other Factors
- Hormonal changes: Hormonal fluctuations, such as those during pregnancy or menopause, can affect blood vessel health and worsen telangiectasia.
- Certain medications: Some medications, like corticosteroids, can weaken blood vessels and contribute to telangiectasia.
- Underlying medical conditions: Conditions like rosacea and scleroderma can worsen telangiectasia.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Hammill AM, Wusik K, Kasthuri RS. Hereditary hemorrhagic telangiectasia (HHT): a practical guide to management. Hematology Am Soc Hematol Educ Program. 2021 Dec 10;2021(1):469-477. doi: 10.1182/hematology.2021000281. PMID: 34889398; PMCID: PMC8791148.
- Sabbà C, Gallitelli M, Pasculli G, Suppressa P, Resta F, Tafaro GE. HHT: a rare disease with a broad spectrum of clinical aspects. Curr Pharm Des. 2006;12(10):1217-20. doi: 10.2174/138161206776361219. PMID: 16611103.
- Rangel-Castilla L, Russin JJ, Martinez-Del-Campo E, Soriano-Baron H, Spetzler RF, Nakaji P. Molecular and cellular biology of cerebral arteriovenous malformations: a review of current concepts and future trends in treatment. Neurosurg Focus. 2014 Sep;37(3):E1. doi: 10.3171/2014.7.FOCUS14214. PMID: 25175428.
- Bofarid S, Hosman AE, Mager JJ, Snijder RJ, Post MC. Pulmonary Vascular Complications in Hereditary Hemorrhagic Telangiectasia and the Underlying Pathophysiology. Int J Mol Sci. 2021 Mar 27;22(7):3471. doi: 10.3390/ijms22073471. PMID: 33801690; PMCID: PMC8038106.




