TL;DR
Elevated lipoprotein(a) [Lp(a)] is an independent risk factor for heart disease and stroke, particularly due to increased blood clot formation.
- Genetic Predominance ▾: Lp(a) levels are primarily determined by genetics.
- Cardiovascular Risk ▾: Elevated Lp(a) is an independent risk factor for heart disease and stroke, particularly due to increased blood clot formation.
- Testing Importance ▾: Testing is crucial, especially for those with a family history of premature cardiovascular disease.
- Limited Lifestyle Impact ▾: Diet and exercise have minimal impact on Lp(a) levels.
- Managing Other Risks ▾: Managing other cardiovascular risk factors (LDL cholesterol, blood pressure) is essential.
*Click ▾ for more information
What is Lipoprotein(a) [Lp(a)]?
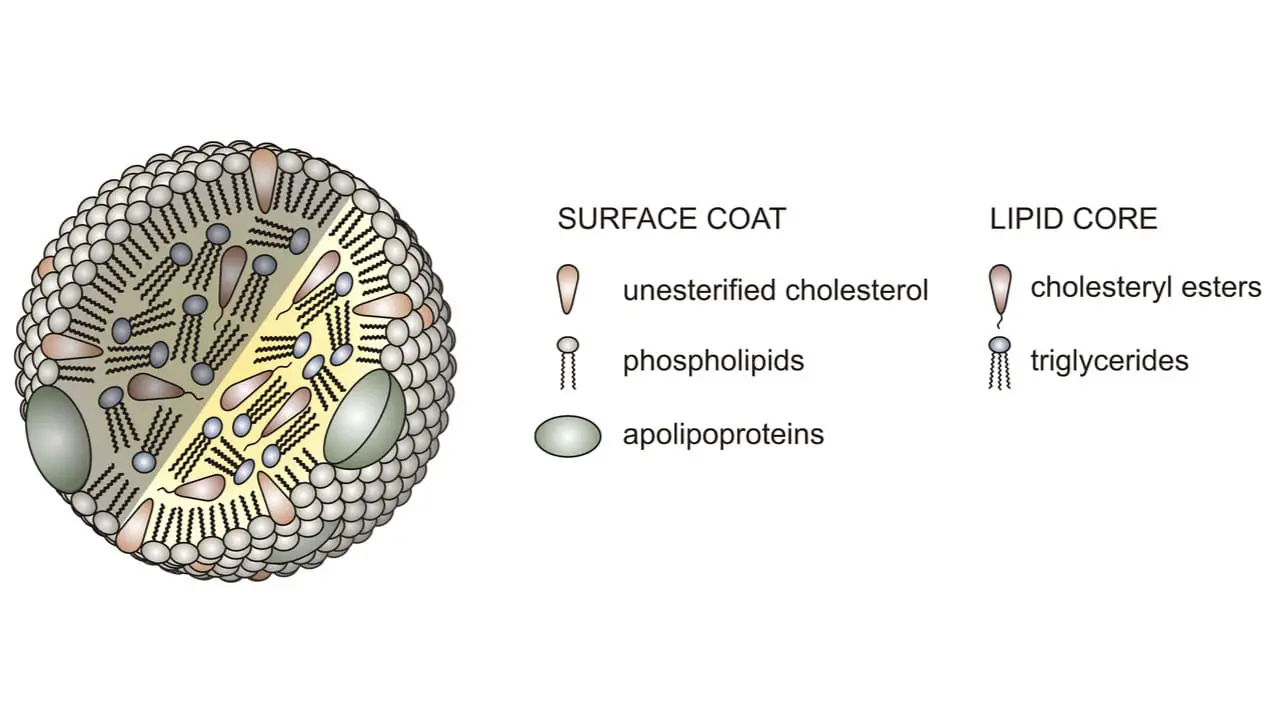
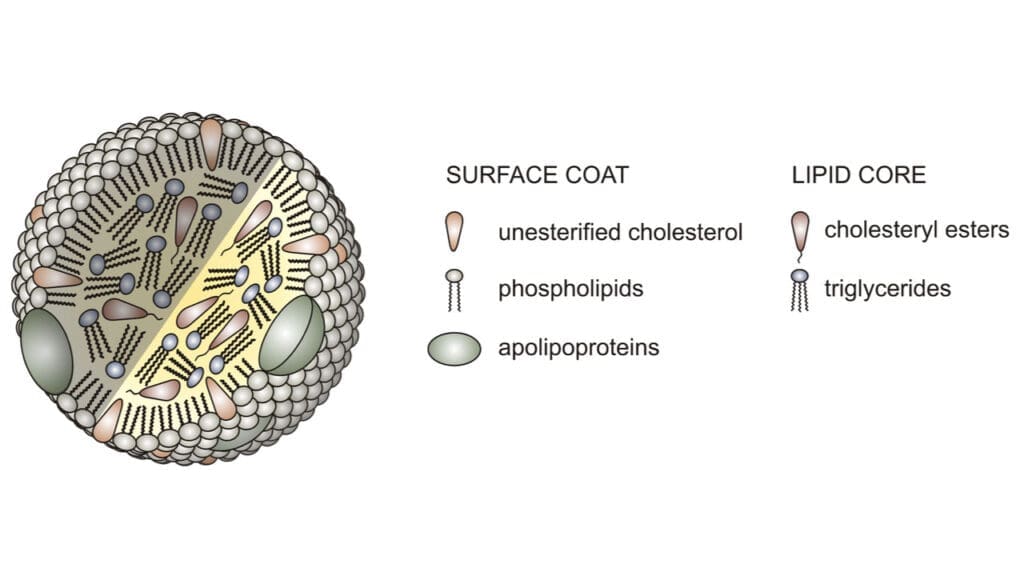
Lipoprotein(a), often shortened to Lp(a), is a type of lipoprotein in your blood.
What it is: Lp(a) is a particle that carries cholesterol through your bloodstream. It’s similar to LDL (“bad”) cholesterol, but it has an extra protein attached to it.
Key feature: That extra protein, called apolipoprotein(a), makes Lp(a) “sticky.” This stickiness can cause Lp(a) to build up in the walls of your arteries.
Why it matters: High levels of Lp(a) increase your risk of developing cardiovascular disease, including:
- Heart attacks
- Strokes
- Aortic stenosis (narrowing of the heart valve)
What is the function of lipoprotein(a) [Lp(a)]?
Understanding the function of Lp(a) is complex, and research is ongoing. While its harmful effects in high concentrations are well-documented, its “normal” physiological role is less clear.
There’s evidence suggesting Lp(a) might play a role in wound healing and tissue repair. Its affinity for fibrin, a protein involved in blood clotting, and its ability to promote cell growth support this theory. Essentially, it may have evolved to aid in the body’s response to injury.
What does a high lipoprotein(a) mean?
A high level of lipoprotein(a) [Lp(a)] in your blood means you have an increased risk of developing cardiovascular disease.
Increased Risk of Atherosclerosis: Lp(a) promotes the buildup of plaque (atherosclerosis) in your artery walls. This plaque can narrow or block arteries, reducing blood flow.
Increased Risk of Blood Clots (Thrombosis): Lp(a) can interfere with your body’s ability to break down blood clots, making you more prone to them. These clots can block blood flow to the heart (heart attack) or brain (stroke).
Increased Risk of Cardiovascular Diseases: Specifically, high Lp(a) is associated with a higher risk of:
- Coronary artery disease (CAD)
- Heart attacks
- Strokes
- Aortic stenosis (narrowing of the heart valve)
- Peripheral artery disease
Independent Risk Factor: It’s crucial to understand that Lp(a) is an independent risk factor. This means it can contribute to heart disease even if your other cholesterol levels (like LDL and HDL) are within a healthy range.
Genetics Play a Large Role: High Lp(a) levels are primarily determined by your genes, so lifestyle changes may not significantly lower them.
In essence, having a high Lp(a) level means your blood is more prone to forming artery-clogging plaque and dangerous blood clots, elevating your overall risk of cardiovascular events.
What causes increase in lipoprotein(a)?
It’s important to understand that lipoprotein(a) [Lp(a)] levels are primarily determined by genetics. However, while genetic factors reign supreme, there are some other influences that can affect Lp(a) levels.
Primary Cause: Genetics
Genetic Inheritance: The most significant factor influencing Lp(a) levels is your genetic makeup. The gene responsible for producing apolipoprotein(a) plays a crucial role. This means that if your parents have high Lp(a) levels, you’re more likely to have them as well.
Other Influencing Factors
- Racial/Ethnic Differences: Studies have shown that certain populations, particularly those of African descent, tend to have higher Lp(a) levels.
- Hormonal Influences: Hormone replacement therapies, and conditions that affect hormone levels such as thyroid disorders, can influence Lp(a) levels. Hormonal changes during menopause can also affect Lp(a) levels.
- Kidney Disease: Chronic kidney disease and nephrotic syndrome have been associated with increased Lp(a) levels.
- Diet: While the effect is less pronounced than with other cholesterol types, some studies indicate that dietary changes can influence Lp(a) levels. Specifically, there is data that shows that replacing saturated fats with carbohydrates, or unsaturated fats, can increase Lp(a) levels.
- Liver conditions: Lp(a) levels are associated with hepatocellular damage.
What is the difference between lipoprotein(a), LDL and cholesterol?
It’s important to understand the distinctions between Lipoprotein(a) [Lp(a)], LDL, and cholesterol, as they all play roles in cardiovascular health, but in distinct ways.
| Feature | Cholesterol | LDL (Low-Density Lipoprotein) | Lipoprotein(a) [Lp(a)] |
| What It Is | Waxy, fat-like substance | Lipoprotein carrying cholesterol | Lipoprotein (LDL + apolipoprotein(a)) |
| Primary Role | Building cells, hormones, vitamin D | Transports cholesterol to cells | Promotes plaque buildup and clotting |
| “Good” or “Bad” | Neither (essential for body functions) | “Bad” cholesterol (in excess) | Highly detrimental (when elevated) |
| Composition | Lipid substance | Cholesterol, proteins, triglycerides | LDL particle + apolipoprotein(a) |
| Key Characteristic | Essential for bodily functions | Contributes to arterial plaque | “Sticky” due to apolipoprotein(a), increases clotting |
| Primary Risk Factor | Not a direct risk factor itself | High levels increase atherosclerosis risk | High levels increase atherosclerosis and thrombosis risk |
| Influenced By | Diet, genetics | Diet, lifestyle, genetics | Primarily genetics |
Who should get tested for lipoprotein(a)?
Lipoprotein(a) [Lp(a)] testing is particularly important for individuals with certain risk factors or family histories.
High-Risk Individuals
- Family History of Premature Cardiovascular Disease: If you have a close relative (parent, sibling, grandparent) who experienced a heart attack, stroke, or other cardiovascular event before age 55 (men) or 65 (women), you should consider Lp(a) testing.
- Personal History of Premature Cardiovascular Disease: Even if your other cholesterol levels are normal, if you’ve had a heart attack, stroke, or other cardiovascular event at a younger age, Lp(a) testing is recommended.
- Familial Hypercholesterolemia (FH): Individuals with FH, a genetic condition that causes high LDL cholesterol, are at increased risk of heart disease and should also have their Lp(a) levels checked.
- Aortic Stenosis: Especially if it develops at a younger than expected age.
- Recurrent cardiovascular events: If someone has had multiple heart attacks, or strokes, even when other risk factors are being well managed.
- People of African Descent: Some studies suggest that individuals of African descent may have naturally higher Lp(a) levels.
Other Considerations
- Individuals with Controlled Risk Factors But Persistent Cardiovascular Events: If you’re managing other risk factors (like high blood pressure, diabetes, and LDL cholesterol) but still experiencing cardiovascular problems, Lp(a) testing might be helpful.
- Those Seeking a Comprehensive Cardiovascular Risk Assessment: Even without specific risk factors, some individuals may choose to get tested for Lp(a) as part of a thorough assessment of their heart health.
In summary, those with a strong family history of early heart disease, or those who have experienced heart events themselves, should highly consider getting tested.
When and how often should lipoprotein(a) be checked?
Lipoprotein(a) [Lp(a)] testing frequency is different from standard cholesterol checks because Lp(a) levels tend to remain relatively stable throughout your life.
When to Get Tested
- Baseline Measurement: For most individuals, a single baseline Lp(a) measurement is sufficient. This is because levels are primarily genetically determined and don’t fluctuate significantly with lifestyle changes. Ideally, this baseline measurement should be done when you are an adult.
- High-Risk Individuals: If you have a strong family history of premature cardiovascular disease, a personal history of premature cardiovascular events, or other risk factors (as discussed previously), testing is highly recommended. Those with familial hypercholesterolemia, or early onset aortic stenosis.
- Following a cardiovascular event: If you have had a heart attack, or stroke, it is recommended to have your Lp(a) levels checked.
How Often to Retest
- Generally, Not Frequently: Because Lp(a) levels are stable, routine retesting is usually not necessary unless there are specific clinical reasons.
- Exceptions: In rare cases, your doctor might recommend retesting if:
- There are significant changes in your health status (e.g., development of kidney disease).
- You’re participating in clinical trials for Lp(a)-lowering therapies.
- There are large changes in hormone levels.
- Guidance from Your Doctor: The frequency of Lp(a) testing should always be determined in consultation with your healthcare provider. They can assess your individual risk factors and provide personalized recommendations.
What is the normal range for lipoprotein(a)?
Generally, Lp(a) levels below 30 mg/dL or 75 nmol/L are considered desirable.
What constitutes a high level of lipoprotein(a)?
Generally, above 30 mg/dL (or 75 nmol/L) is considered elevated.
However, many experts consider levels above 50 mg/dL (or ~125 nmol/L) to be significantly high and associated with a substantially increased risk.
Levels exceeding 100 mg/dL (or ~250 nmol/L) are considered very high and pose a particularly significant cardiovascular risk.
Associated Risks of High Lp(a)
- Atherosclerosis: Lp(a) contributes to the buildup of plaque in the artery walls, which narrows the arteries and restricts blood flow.
- Thrombosis (Blood Clots): Lp(a) interferes with the body’s natural ability to dissolve blood clots, increasing the risk of clots forming in the arteries.
- Coronary Artery Disease (CAD): High Lp(a) significantly elevates the risk of CAD, which can lead to angina (chest pain) and heart attacks.
- Heart Attacks (Myocardial Infarction): Plaque buildup and blood clots caused by high Lp(a) can block blood flow to the heart, resulting in a heart attack.
- Strokes (Cerebrovascular Accident): Similarly, blockages in arteries leading to the brain can cause strokes.
- Aortic Stenosis: Lp(a) has been linked to the calcification (hardening) of the aortic valve, leading to aortic stenosis, a narrowing of the heart valve.
- Peripheral Artery Disease (PAD): High Lp(a) increases the risk of plaque buildup in the arteries of the legs and feet, causing PAD.
- Increased risk of recurrent cardiovascular events: Those with high Lp(a) have an increased risk of having a second, or third cardiovascular event.
How do you test for lipoprotein(a)?
The test for lipoprotein(a) [Lp(a)] is a relatively straightforward blood test. In many cases, you’ll be asked to fast for 9 to 12 hours before the test. This means not eating or drinking anything other than water. A lipoprotein(a) test measures the level of Lp(a) in your blood. It’s a standard blood draw, where a healthcare professional takes a blood sample from a vein in your arm. The blood sample is then sent to a laboratory for analysis.
Recommended Test for Lipoprotein(a)
empowerDx Lp(a)-Lipoprotein(a) Test – At home test kit
- Tests for: This kit measures the concentration of lipoprotein(a) [Lp(a)] in your blood. This provides a quantitative result indicating your Lp(a) level, typically expressed in milligrams per deciliter (mg/dL).
- How it works: Buy a kit from Amazon.com and follow the instructions on the kit.
- Specimen required: Finger prick blood sample
- Results in: 4 – 7 days after shipping.
About the test
The empowerDX lipoprotein(a) test kit measures Lp(a) levels using a finger-prick blood sample, providing quantitative results typically within days to a week. It’s crucial to follow kit instructions, including potential fasting requirements, ensure proper hygiene, and discuss results with a healthcare provider for accurate interpretation and to manage any associated cardiovascular risk.
| Pros | Cons |
|---|---|
| ✅ Easy to use ✅ Clear instructions ✅ CLIA-Certified Labs | ❌ Need to do finger prick using a lancet ❌ User error in sample collection or handling can affect results. ❌ Test is slightly expensive |
Disclaimer: This information is based on research and is accurate to the best of our knowledge at the time of publication. Please note that the writer has not personally used or tested these products.
How is high lipoprotein(a) treated?
Currently, there is no specific cure or treatment for high lipoprotein(a). However, there are several strategies recommended by physicians.
Current Strategies
- Lifestyle Modifications: While lifestyle changes don’t directly lower Lp(a) levels, they’re crucial for managing overall cardiovascular risk. This includes:
- Maintaining a healthy weight.
- Regular physical activity.
- A heart-healthy diet.
- Avoiding tobacco.
- Managing other risk factors like high blood pressure and diabetes.
- Lowering LDL Cholesterol: Since Lp(a) is a type of LDL cholesterol, lowering overall LDL levels is important. Medications like statins and PCSK9 inhibitors can help. It is important to note that statins can slightly raise Lp(a) levels, but their benefits in lowering LDL and reducing cardiovascular risk generally outweigh this.
- Lipoprotein Apheresis: This is a procedure similar to dialysis that removes Lp(a) from the blood. It’s typically reserved for individuals with very high Lp(a) levels and other significant risk factors, such as familial hypercholesterolemia.
Frequently Asked Questions (FAQs)
What is the best way to lower lipoprotein(a)?
It’s important to understand that lipoprotein(a) [Lp(a)] levels are primarily determined by genetics, making them less responsive to lifestyle changes compared to other cholesterol markers. However, there are strategies to manage Lp(a) and reduce the associated cardiovascular risk.
Key Approaches
Focus on Overall Cardiovascular Risk Reduction
Since directly lowering Lp(a) can be challenging, a strong emphasis is placed on minimizing other modifiable risk factors. This includes:
- Managing LDL Cholesterol: Lowering “bad” LDL cholesterol with statins or PCSK9 inhibitors is crucial. While statins might slightly increase Lp(a), their overall benefit in reducing cardiovascular risk outweighs this. PCSK9 inhibitors are noted to reduce both LDL and Lp(a) levels.
- Controlling Blood Pressure: Maintaining healthy blood pressure is vital.
- Managing Diabetes: If you have diabetes, strict blood sugar control is essential.
- Healthy Lifestyle:
- A heart-healthy diet.
- Regular physical activity.
- Avoiding tobacco.
- Maintaining a healthy weight.
Medications
- Niacin: This vitamin can lower Lp(a), but it can also cause side effects, so it’s not always the first choice.
- PCSK9 Inhibitors: These medications, while primarily used to lower LDL cholesterol, also have a beneficial effect on Lp(a) levels.
- Emerging Therapies: New medications specifically targeting Lp(a), such as siRNA therapies, are showing promising results in clinical trials. These represent a significant advancement in Lp(a) management.
- Lipoprotein Apheresis: This procedure, similar to dialysis, physically removes Lp(a) from the blood. It’s reserved for high-risk individuals with very elevated Lp(a) levels.
Important Considerations
- Lp(a) testing is crucial for identifying individuals at increased risk.
- Treatment decisions should be individualized, based on your overall cardiovascular risk profile.
- Consulting with a cardiologist or lipid specialist is recommended for personalized guidance.
- It is very important to keep up to date with the latest research into Lp(a) lowering medications, as this area of research is very active.
Can I live a long life with high lipoprotein(a)?
Living a long life with high lipoprotein(a) [Lp(a)] is possible, but it requires proactive management of cardiovascular risk.
High Lp(a) is an independent risk factor for cardiovascular disease, meaning it increases the likelihood of heart attacks, strokes, and other related problems. The level of increased risk varies from individual to individual.
Managing the Risks
- Aggressive Management of Other Risk Factors: This is crucial. Even if you can’t significantly lower your Lp(a), you can control other modifiable risk factors like:
- LDL cholesterol: Keep it low through diet, exercise, and medication if necessary.
- Blood pressure: Maintain healthy blood pressure levels.
- Diabetes: If you have diabetes, strict blood sugar control is essential.
- Lifestyle: Adopt a heart-healthy lifestyle, including a balanced diet, regular exercise, and no smoking.
- Medical Interventions: Your doctor may recommend medications or procedures to lower your overall cardiovascular risk. Emerging Lp(a)-lowering therapies are also becoming available, which could significantly improve outcomes.
- Regular Monitoring: Regular checkups with your doctor are essential to monitor your Lp(a) levels and overall cardiovascular health.
Can exercise lower lipoprotein(a)?
While exercise is vital for cardiovascular health, it doesn’t significantly lower lipoprotein(a) [Lp(a)] levels, which are primarily genetically determined; however, regular physical activity is still crucial for managing other cardiovascular risk factors like LDL cholesterol, blood pressure, and weight, thus contributing to overall well-being even with elevated Lp(a).
Why don’t doctors test for lipoprotein(a)?
Lipoprotein(a) testing isn’t routine due to factors like the historical lack of specific treatments, evolving clinical guidelines, and the fact that it’s often reserved for those with specific risk factors like a family history of premature heart disease, though increased awareness and new therapies are leading to more frequent testing, especially in high-risk individuals.
Do statins lower lipoprotein(a)?
Statins generally do not lower lipoprotein(a) [Lp(a)] levels. In fact, some studies have shown that statins can slightly increase Lp(a) levels. However, statins are still very important for people with high Lp(a) because they effectively lower LDL cholesterol, which significantly reduces overall cardiovascular risk.
Does lipoprotein(a) increase with age?
Generally, lipoprotein(a) [Lp(a)] levels are considered to be relatively stable throughout adulthood and are primarily determined by genetics. While there might be minor fluctuations, a significant increase with age is not typically observed.
Therefore, while age itself may not cause a significant increase in Lp(a) levels, the accumulated risk from having high Lp(a) levels does increase as you get older.
Can stress cause high lipoprotein(a)?
Stress does not directly cause high lipoprotein(a) [Lp(a)] levels, which are primarily genetic, but chronic stress can heighten cardiovascular risks by influencing factors like blood pressure and lifestyle choices, thus indirectly increasing the likelihood of cardiovascular events in individuals with pre-existing elevated Lp(a).
Can lipoprotein(a) cause a stroke?
Yes, elevated lipoprotein(a) [Lp(a)] is an independent risk factor for stroke, particularly ischemic stroke (caused by a blood clot).
What are the best foods to lower lipoprotein(a)?
It’s important to clarify that while diet plays a significant role in overall cardiovascular health, directly lowering lipoprotein(a) [Lp(a)] levels through food alone is challenging, as Lp(a) is primarily genetically determined. However, a heart-healthy diet can significantly reduce other cardiovascular risk factors, which is crucial for individuals with elevated Lp(a).
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Lampsas S, Xenou M, Oikonomou E, Pantelidis P, Lysandrou A, Sarantos S, Goliopoulou A, Kalogeras K, Tsigkou V, Kalpis A, Paschou SA, Theofilis P, Vavuranakis M, Tousoulis D, Siasos G. Lipoprotein(a) in Atherosclerotic Diseases: From Pathophysiology to Diagnosis and Treatment. Molecules. 2023 Jan 18;28(3):969. doi: 10.3390/molecules28030969. PMID: 36770634; PMCID: PMC9918959.
- Kamstrup PR. Lipoprotein(a) and Cardiovascular Disease. Clin Chem. 2021 Jan 8;67(1):154-166. doi: 10.1093/clinchem/hvaa247. PMID: 33236085.
- Schmidt K, Noureen A, Kronenberg F, Utermann G. Structure, function, and genetics of lipoprotein (a). J Lipid Res. 2016 Aug;57(8):1339-59. doi: 10.1194/jlr.R067314. Epub 2016 Apr 13. PMID: 27074913; PMCID: PMC4959873.
- Alhomoud IS, Talasaz A, Mehta A, Kelly MS, Sisson EM, Bucheit JD, Brown R, Dixon DL. Role of lipoprotein(a) in atherosclerotic cardiovascular disease: A review of current and emerging therapies. Pharmacotherapy. 2023 Oct;43(10):1051-1063. doi: 10.1002/phar.2851. Epub 2023 Jul 26. PMID: 37464942.