Introduction
Blood transfusions are life-saving medical procedures, but incompatible blood types can lead to severe and potentially fatal reactions. To ensure safety, we rely on a meticulous process of antibody identification, and a key tool in this process is the antibody identification antigram. This introduction delves into the principle, methodology, and interpretation of antigrams, empowering you to decipher the cryptic messages they hold and select compatible red blood cells for transfusion.
Principle of Antigram Interpretation
The principle behind antigram interpretation hinges on the intricate relationship between antibodies and antigens. Antibodies, also known as immunoglobulins, are specialized proteins produced by our immune system in response to foreign invaders. These antibodies have a unique ability to recognize and bind to specific structures on the surface of cells, known as antigens. In the context of blood transfusions, red blood cells (RBCs) can display a diverse array of antigens on their surface, categorized into different blood group systems. If an individual is exposed to foreign RBCs through transfusion or pregnancy, their immune system can generate antibodies against these mismatched antigens.
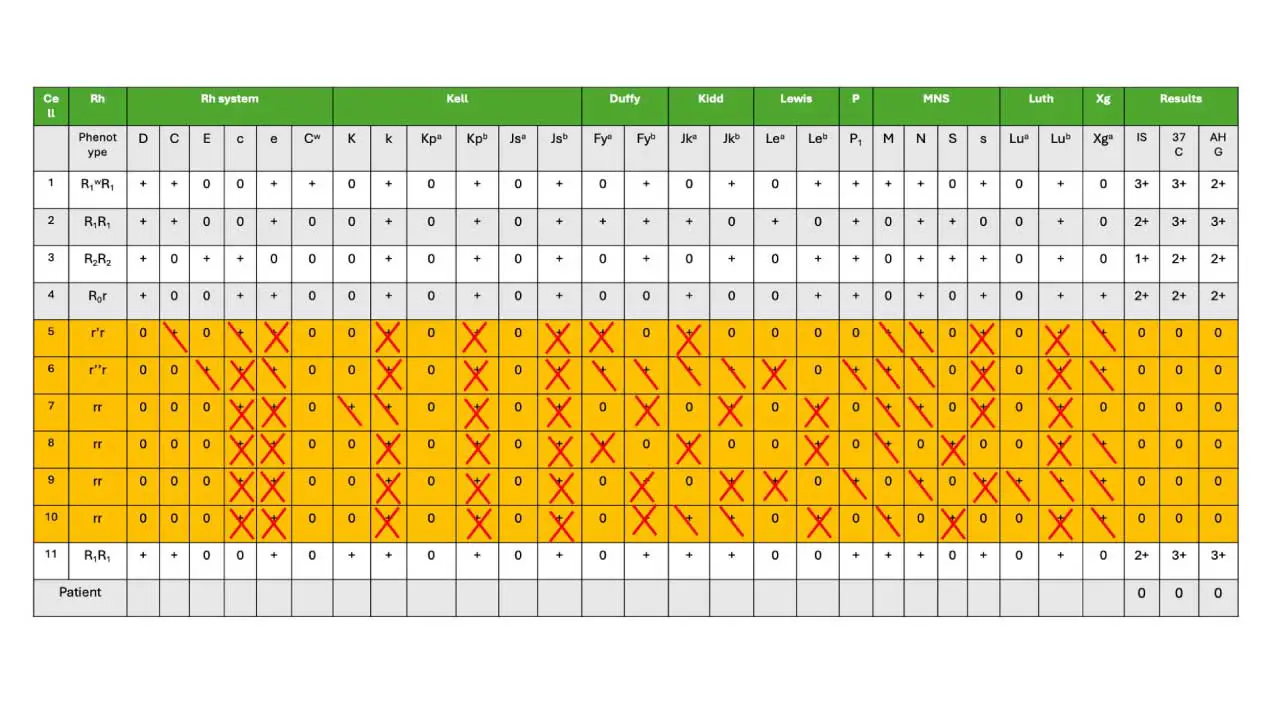
The methodology of antibody identification involves a series of tests using an antibody panel. This panel consists of a collection of well-defined RBCs, each possessing a known profile of antigens. The recipient’s serum or plasma is then incubated with each cell type in the panel. The antigram, a document accompanying the panel, acts as a decoder ring for these interactions. It meticulously lists the antigens present (denoted by “+”) and absent (“0”) on each RBC in the panel. Following incubation, the presence of agglutination (clumping) of RBCs indicates a positive reaction, signifying an antibody-antigen interaction. The results are meticulously recorded on the antigram, transforming it from a static document to a personalized roadmap for antibody identification.
Interpretation of the antigram is an intellectual puzzle, demanding a keen eye and a logical approach. We begin by analyzing the positive reactions. Look for commonalities among the reactive cells – which antigens do they all possess? This points towards the potential antigen targeted by the recipient’s antibody. However, this is just the first step. Ruling out other possibilities is crucial. We utilize the negative reactions – cells that did not react with the recipient’s serum. These cells likely lack the suspected antigen, and their corresponding antigens on the antigram can be excluded from the culprit.
Through a meticulous process of inclusion and exclusion, the antigram unveils the identity of the antibody. This newfound knowledge empowers us to select compatible blood for transfusion. By choosing donor RBCs that demonstrably lack the antigen targeted by the recipient’s antibody, we can prevent a potentially devastating transfusion reaction. The antigram thus serves as a vital bridge between the recipient’s immune response and the selection of safe and compatible blood for transfusion.
Interpretation Method
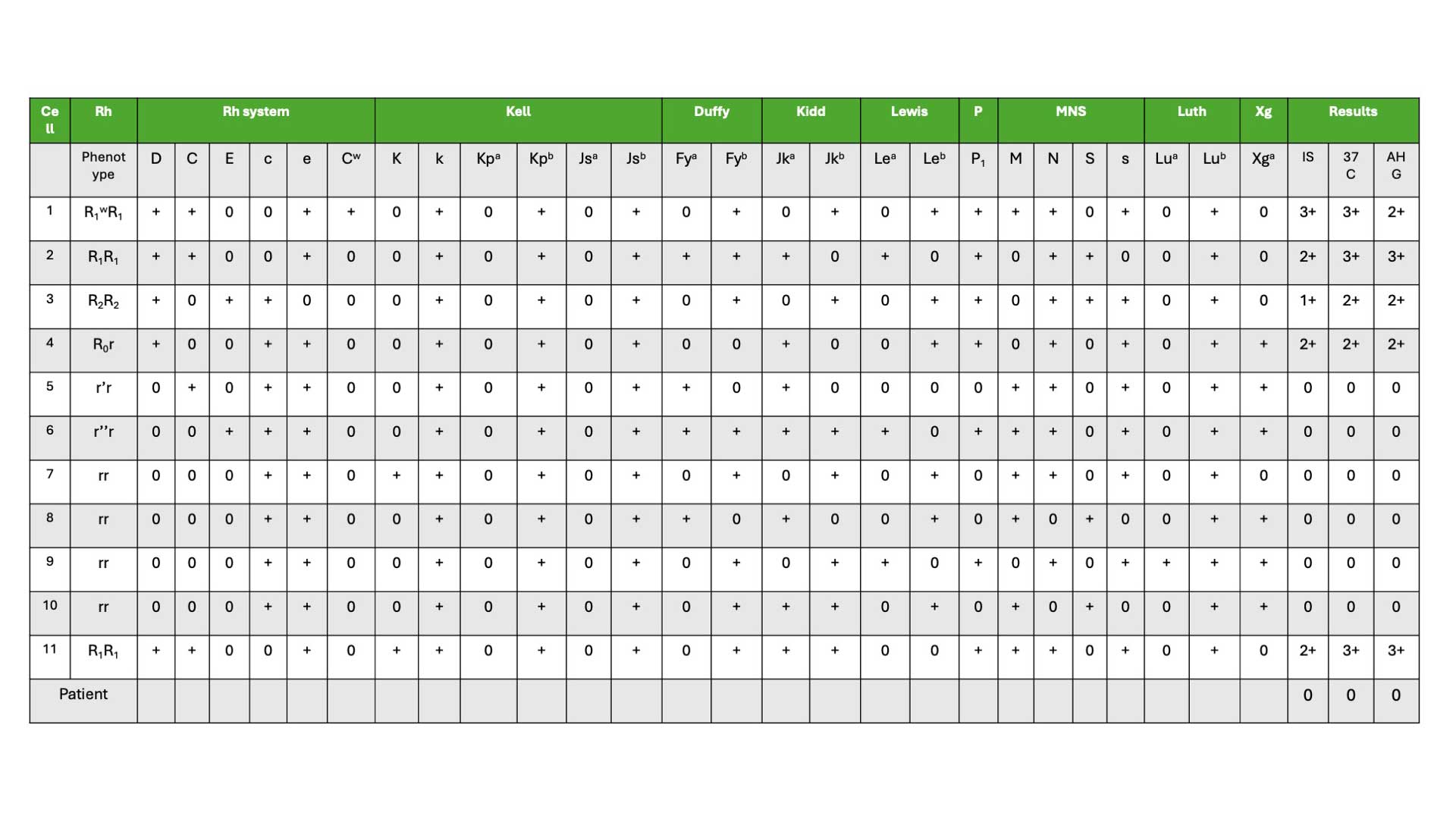
- Identify the RBCs that show a negative result (0) or no reaction in all steps of the antibody identification process. This is seen in cells 5 – 10 in our antigram example.
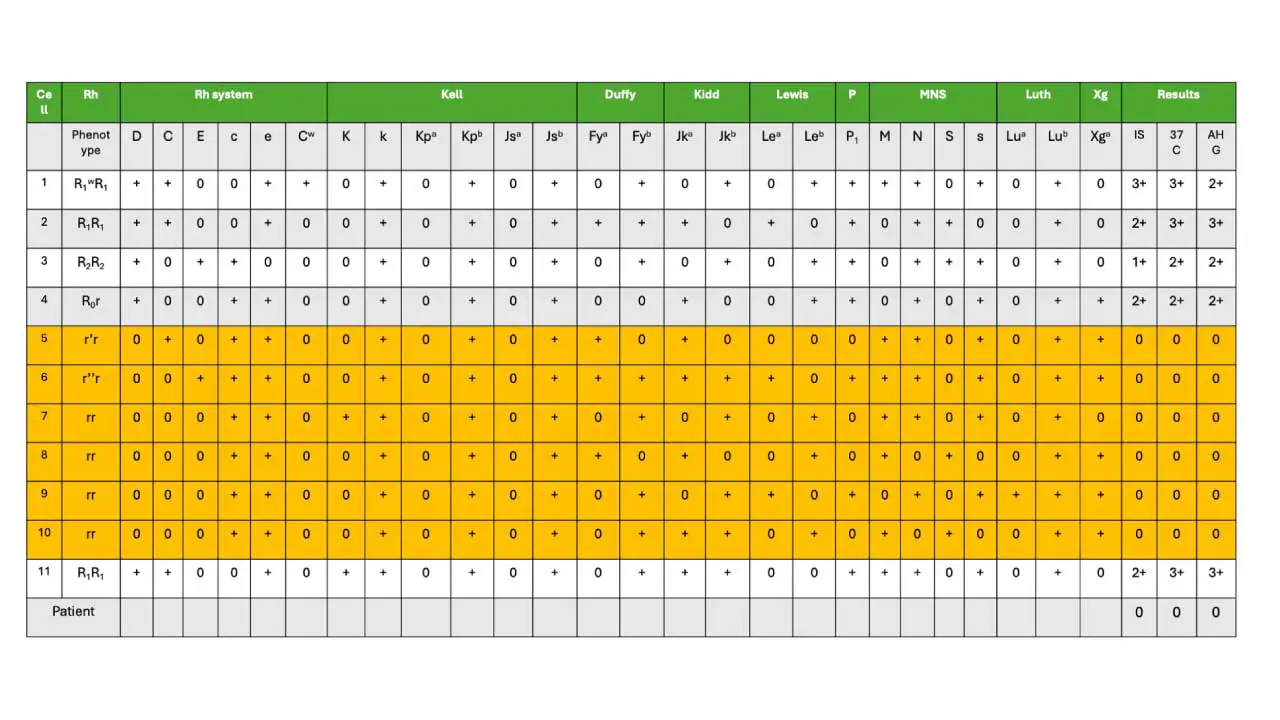
2. Analyze each cell line from the rows above and identify antigens listed as “+”. For each antigen, mark it as follows:
- If the antigen is likely present in both copies of the recipient’s red blood cells (homozygous), mark it with an “X”.
- If the antigen is present in only one copy of the recipient’s red blood cells (heterozygous), mark it with a “/”.
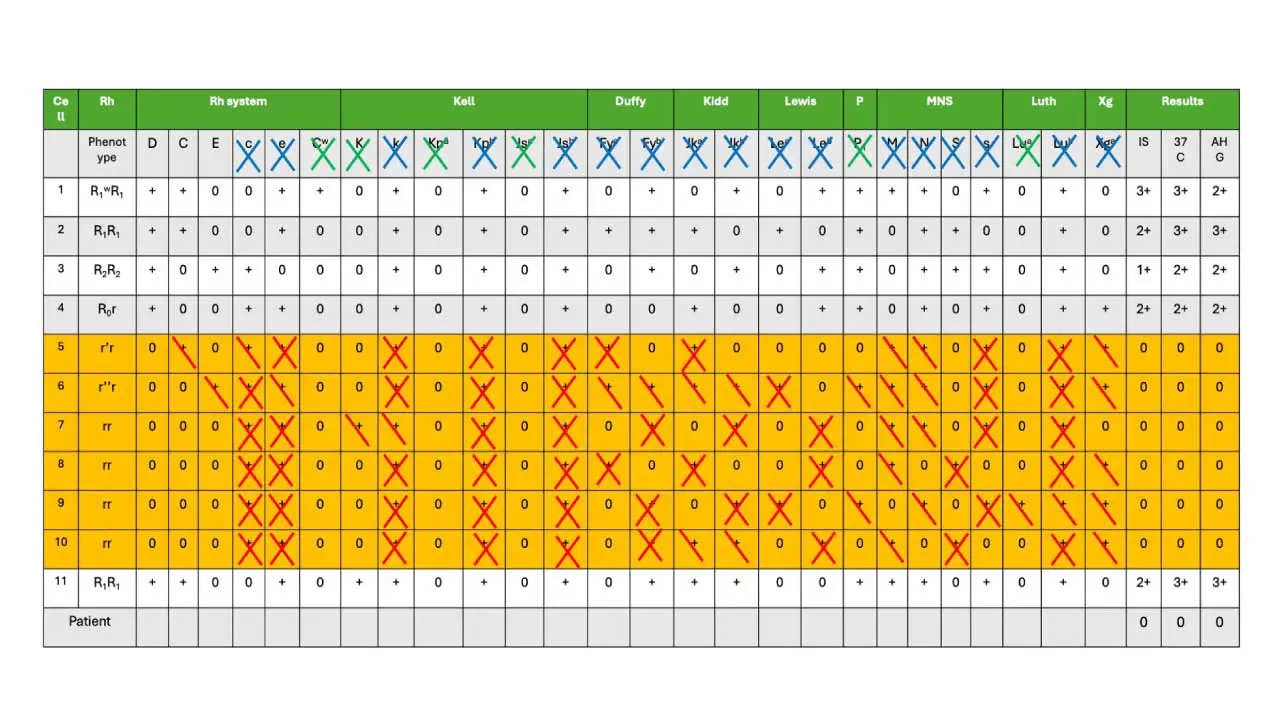
3. To identify the antibody specificity, exclude antigens that appear crossed out (“X” or “/”) three or more times on the antigram. Ideally, at least one of these excluded antigens should be marked with an “X” (indicating it’s present on both copies of the red blood cell). This suggests a stronger likelihood that the antibody targets this specific antigen. In our antigram example, these are marked as blue X at the top of the panel.
Low frequency or rare antigens can also be crossed off (marked as green X at the top of the panel). These include Cw, Kpa, Jsa, K, Lua, P1.
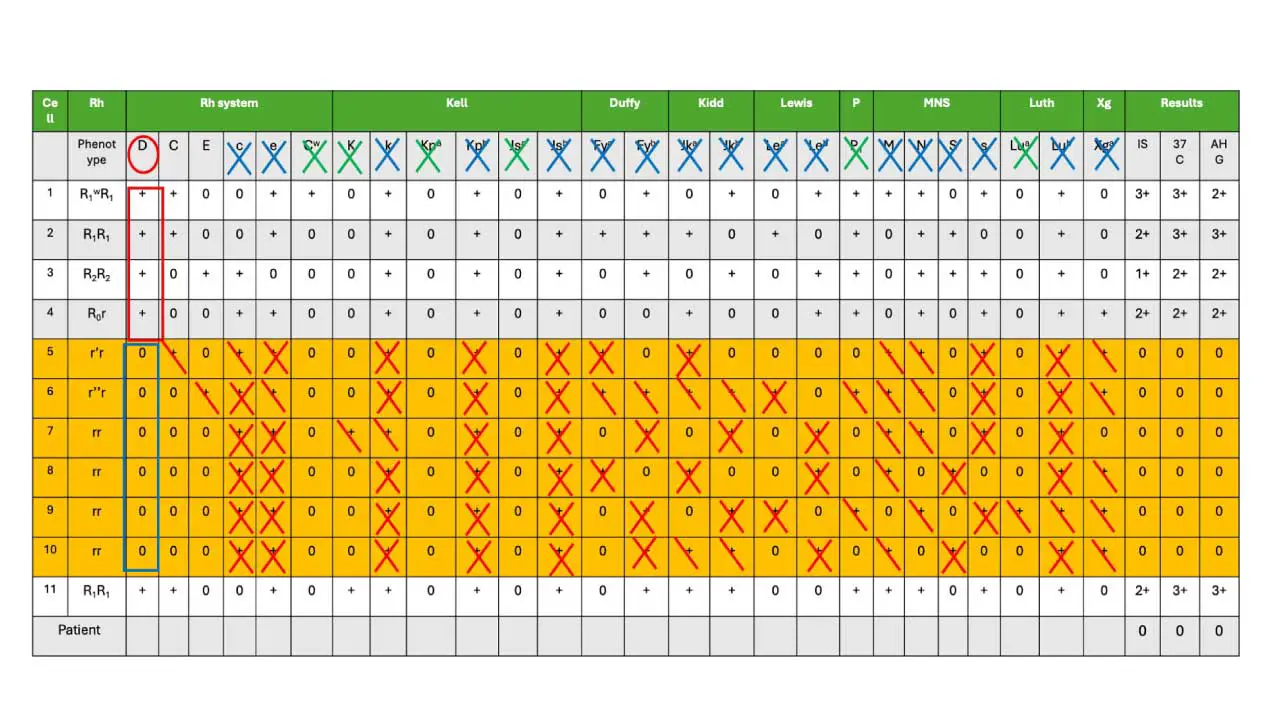
To confirm that the antibody identified is anti-D, the following criteria must be fulfilled:
- Positive Reactions (Red Box): We need at least three red blood cells (RBCs) with the suspected antigen to be present and show a positive reaction (+) with the recipient’s serum/plasma (marked in the red box).
- Negative Reactions (Blue Box): We also need at least three RBCs lacking the suspected antigen to exhibit a negative reaction (0) with the recipient’s serum/plasma (marked in the blue box in cells 5-10).
- Clinically Significant Antibodies: It’s crucial to exclude common clinically significant antibodies like RhD, Duffy, MNSs, P, Kell, Kidd, and Lewis system antibodies through additional testing before concluding the antibody identification.
Antigram Result
The presence of the anti-D antibody (anti-D positive) is strongly suggested based on two key observations:
- Negative Autocontrol (AC): The autocontrol test, which uses the recipient’s own red blood cells, is negative. This indicates the absence of self-directed antibodies (autoantibodies) that could potentially complicate the interpretation of the results.
- Anti-D Explains Reactions: The reactivity pattern observed in the antibody identification panel can be fully explained by the presence of anti-D. This means all the positive reactions in the panel are consistent with the expected behavior of anti-D binding to specific antigens on the test red blood cells.
Additional Considerations
- While anti-D is the most likely culprit, the possibility of other antibodies, particularly those targeting low-frequency antigens, cannot be entirely ruled out at this stage.
- Further testing may be necessary to definitively identify any additional antibodies, especially if the transfusion history suggests potential exposure to other blood group antigens.
- Ensure consistency between the antibody screen and identification results. This is a crucial quality control step to verify the antibody identification reflects the actual antibodies present in the recipient’s sample and minimizes the risk of transfusing incompatible blood due to a sample mix-up.
Dosage Effect
The dosage effect can complicate the interpretation of antibody identification panels. Sometimes, an antibody might only react strongly enough to be detected with RBCs that have the double dose of the target antigen. This could lead to a false negative result (no reaction) with RBCs that have the single dose.
Here’s an example:
- Imagine an antibody against antigen “A.”
- RBCs from person 1 have a single dose of antigen A (heterozygous).
- RBCs from person 2 have a double dose of antigen A (homozygous).
- The antibody might react strongly with person 2’s RBCs (causing agglutination) but show a weak or negative reaction with person 1’s RBCs, even though they both possess the antigen A.
Therefore, it’s important to be aware of the dosage effect when interpreting antibody identification panels. Examples of blood group systems that exhibit the dosage effect include Rh, Kidd, and Duffy. When testing for antibodies in these systems, it’s crucial to consider the dosage effect to avoid misinterpreting weak or negative reactions with heterozygous RBCs. If a weak or negative reaction is observed, further testing might be necessary to confirm the presence of the antibody.
Disclaimer: This protocol is intended for informational purposes only and may need to be modified depending on the specific laboratory procedures and patient circumstances. Always consult with a qualified healthcare professional for guidance. See additional information.
References
- American Association of Blood Banks (AABB). Technical Manual, 21st Edition, 2023.
- Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005.
- Bain BJ, Bates I, Laffan MA. Dacie and Lewis Practical Haematology: Expert Consult: Online and Print 12th Edition (Elsevier). 2016.
- International Society of Blood Transfusion. https://www.isbtweb.org/resources/resources-library.html
- British Committee for Standards in Haematology, C. Milkins, J. Berryman, C. Cantwell, C. Elliott, R. Haggas, J. Jones, M. Rowley, M. Williams, N. Win (2013). Guidelines for pre-transfusion compatibility procedures in blood transfusion laboratories. Transfusion Medicine. 2023(1): 3-35.
- Knowles, S.M., Milkins, C.E., Chapman, J.F. & Scott, M. (2002) The United Kingdom National External Quality Assessment Scheme (blood transfusion laboratory practice): trends in proficiency and practice between 1985 and 2000. Transfusion Medicine, 12, 11–23.
- SHOT (1996–2010) Serious Hazards of Transfusion annual reports. (Accessed 31/05/24).