TL;DR
Eosinophilic esophagitis (EoE) is a chronic, immune/antigen-mediated esophageal disease. It’s characterized by eosinophil-predominant inflammation.
- Increasing prevalence, particularly in children and young adults.
- Male predominance.
- Linked to atopic conditions.
- Th2-mediated immune response.
- Key cytokines: IL-4, IL-5, IL-13.
- Food and environmental allergens are primary triggers.
- Genetic predisposition plays a large role.
- Esophageal remodeling leads to fibrosis and strictures.
- Adults: Dysphagia, food impaction, chest pain.
- Children: Feeding difficulties, abdominal pain, vomiting.
- Endoscopy with multiple biopsies (≥15 eosinophils/HPF).
- Histopathology: eosinophilic microabscesses, basal cell hyperplasia, dilated intercellular spaces.
- Allergy testing to identify triggers.
- Differentiate from GERD, achalasia, Crohn’s disease, and other esophageal disorders.
- Dietary therapy (elimination diets).
- Topical corticosteroids (fluticasone, budesonide).
- Proton pump inhibitors (PPIs).
- Biologics (Dupilumab).
- Endoscopic dilation for strictures.
- Food impaction.
- Esophageal strictures.
- Esophageal perforation (rare).
- Decreased quality of life.
- Chronic condition requiring long-term management.
- Good prognosis with adherence to treatment.
- Early diagnosis is crucial.
*Click ▾ for more information
Introduction
Eosinophilic esophagitis (EoE) is a chronic, immune/antigen-mediated esophageal disease characterized by inflammation driven by an accumulation of eosinophils within the esophageal mucosa. Unlike gastroesophageal reflux disease (GERD), where eosinophils may be present in small numbers due to acid irritation, eosinophilic esophagitis (EoE) is defined by a significant and persistent eosinophilic infiltration. This inflammatory process results in esophageal dysfunction, leading to a variety of clinical symptoms.
Significance
EoE is increasingly recognized as a significant cause of esophageal morbidity, particularly in children and young adults. The prevalence of eosinophilic esophagitis (EoE) has been steadily rising over the past few decades, likely due to increased awareness, improved diagnostic techniques, and potentially, environmental factors.
Understanding eosinophilic esophagitis (EoE) is crucial for medical practitioners as it requires a distinct diagnostic and management approach compared to other esophageal disorders.
The quality of life of patients with eosinophilic esophagitis (EoE) can be severely impacted, so early diagnosis and treatment is very important.
Epidemiology
Prevalence and incidence
Eosinophilic esophagitis (EoE) is considered a relatively common esophageal disorder, although precise prevalence figures are challenging due to variations in diagnostic criteria and access to healthcare.
Estimates of prevalence range from approximately 10 to 50 cases per 100,000 individuals, but these numbers are likely underestimated. The incidence of eosinophilic esophagitis (EoE) is also increasing, reflecting greater awareness and improved diagnostic capabilities.
Demographics
Eosinophilic esophagitis (EoE) can affect individuals of all ages, but it is more commonly diagnosed in children and young adults. There is a significant male predominance, with males being affected approximately 2-4 times more often than females. The reason for this sex disparity is not fully understood. While eosinophilic esophagitis (EoE) is observed in various racial and ethnic groups, studies suggest a higher prevalence in Caucasian populations.
Geographic distribution
Eosinophilic esophagitis (EoE) has been reported worldwide, but there appear to be regional variations in prevalence. Higher rates have been observed in developed countries, particularly in North America and Europe. This may reflect differences in environmental exposures, dietary habits, or access to diagnostic services. Environmental factors such as climate, and aeroallergen exposure may play a role in geographical distribution.
Pathogenesis of Eosinophilic Esophagitis (EoE)
Eosinophilic esophagitis (EoE) is fundamentally an immune-mediated disease, with a strong emphasis on Th2-type inflammation. Th2 lymphocytes play a central role in orchestrating the inflammatory response. Upon exposure to allergens (primarily food), Th2 cells release a cascade of cytokines that drive eosinophil recruitment and activation.
Cytokines and chemokines that are involved in EoE include:
- IL-4: Promotes Th2 differentiation and IgE production.
- IL-5: Crucial for eosinophil maturation, recruitment, and survival.
- IL-13: Induces eotaxin-3 production by epithelial cells, contributing to eosinophil chemotaxis, as well as promoting epithelial barrier dysfunction.
- Eotaxin-3: This chemokine is a key driver of eosinophil recruitment to the esophagus. It is upregulated in EoE, particularly in response to IL-13.
These and other cytokines contribute to the inflammatory cascade, leading to the characteristic eosinophilic infiltration of the esophageal mucosa. This chronic inflammation in eosinophilic esophagitis (EoE) then leads to structural changes in the esophagus.
Repeated cycles of inflammation and tissue repair result in the deposition of collagen and other extracellular matrix components, leading to fibrosis. Fibrosis can cause esophageal narrowing and stricture formation, contributing to dysphagia and food impaction. Esophageal motility can be impaired in eosinophilic esophagitis (EoE), further contributing to swallowing difficulties.
The esophageal epithelial barrier is vital for preventing the penetration of antigens. In eosinophilic esophagitis (EoE), this barrier is often compromised, allowing increased permeability to allergens. This dysfunction is driven by cytokines like IL-13, and contributes to the ongoing inflammatory response. Dilated intercellular spaces are a histological hallmark of this dysfunction.
Causes and Risk Factors
Food Allergens
These are the most significant triggers for EoE. The reaction is typically a delayed hypersensitivity, not an immediate IgE-mediated allergy.
Common food triggers include:
- Milk (dairy)
- Wheat
- Soy
- Eggs
- Peanuts
- Tree nuts
- Seafood
Identifying specific food triggers can be challenging, often requiring elimination diets and allergy testing.
Environmental Allergens
Aeroallergens can exacerbate eosinophilic esophagitis (EoE) symptoms.
Common environmental triggers:
- Pollen
- Dust mites
- Animal dander
The role of environmental allergens may explain seasonal variations in EoE symptoms.
Genetic Factors
Eosinophilic esophagitis (EoE) has a strong genetic component, as evidenced by familial clustering and association with specific gene variants.
- TSLP (Thymic Stromal Lymphopoietin): This gene encodes a cytokine that initiates Th2 immune responses. Variations in TSLP may increase susceptibility to eosinophilic esophagitis (EoE) by promoting eosinophilic inflammation.
- FLG (Filaggrin): This gene encodes a protein crucial for maintaining the skin and esophageal epithelial barrier. Mutations in FLG can lead to barrier dysfunction, increasing permeability to allergens and contributing to eosinophilic esophagitis (EoE) development. This gene is also heavily implicated in Atopic dermatitis, which is a common comorbidity.
The genetic component helps to explain why some individuals develop eosinophilic esophagitis (EoE) in response to allergens, while others do not. Atopic conditions such as asthma, eczema, and allergic rhinitis are risk factors, and share some genetic links with eosinophilic esophagitis (EoE). Family history of eosinophilic esophagitis (EoE) or other atopic diseases increases the risk.
Male Predominance
Eosinophilic esophagitis (EoE) is more common in males than females. The reason for this sex disparity is not fully understood. Hormonal influences and sex-specific differences in immune responses may play a role.
Pediatric vs. Adult Presentation Differences
Children are more likely to present with feeding difficulties, abdominal pain, and vomiting. Adults typically experience dysphagia, food impaction, and chest pain.
Clinical Presentation and Symptoms of EoE
Eosinophilic esophagitis (EoE) symptoms can vary significantly between individuals, and some patients may be asymptomatic or have only mild symptoms. The overlap of symptoms with other esophageal disorders, such as GERD and achalasia, can make diagnosis challenging. It is crucial to consider EoE in patients with persistent dysphagia or other esophageal symptoms, even if they have a history of GERD.
Symptoms in Adults
- Dysphagia (Solid Food): This is the hallmark symptom in adults. Difficulty swallowing solid foods, particularly dry or dense foods like bread or meat, is very common.
- Food Impaction: Episodes of food getting lodged in the esophagus, requiring emergency intervention, are frequent and distressing. This is a key distinguishing symptom.
- Chest Pain: Non-cardiac chest pain, often described as a burning or squeezing sensation, can occur. This can sometimes be confused with cardiac chest pain.
- Heartburn/Reflux-like Symptoms: While EoE is distinct from GERD, some patients may experience heartburn, regurgitation, or other reflux-like symptoms. It’s important to note that these symptoms are due to esophageal dysfunction caused by eosinophilic inflammation, not necessarily acid reflux.
- Upper abdominal pain
- “Compensatory eating behaviors”: Some patients will modify their diet, eating only soft foods, or eating very slowly, in order to avoid symptoms.
Symptoms in Children
- Feeding Difficulties: Infants and young children may exhibit poor feeding, food refusal, or selective eating.
- Abdominal Pain: This is a common complaint, often described as a vague or diffuse discomfort.
- Vomiting: Frequent vomiting or regurgitation can occur, particularly after meals.
- Failure to Thrive: In severe cases, chronic inflammation and reduced food intake can lead to poor growth and weight gain.
- Reflux like symptoms
- Irritability around meal times
Children with eosinophilic esophagitis (EoE) may develop learned food avoidance behaviors due to negative experiences with eating. They may become anxious or fearful around mealtimes, leading to further feeding difficulties. These behavioral changes can significantly impact their quality of life and nutritional status. Children may learn to drink excessive amounts of fluids with their meals to help with swallowing.
Laboratory Investigations and Diagnostic Procedures
Endoscopy
This is the cornerstone of eosinophilic esophagitis (EoE) diagnosis.
- Visual Findings:
- Esophageal Furrows: Linear or circular grooves running along the esophageal mucosa.
- Esophageal Rings: Concentric, fixed rings that narrow the esophageal lumen.
- White Plaques/Specks: Small, raised white areas representing eosinophil aggregates.
- Crepe Paper Esophagus: A fragile, corrugated appearance of the esophageal mucosa.
- Edema: Swelling of the esophageal walls.
These visual findings, while suggestive, are not pathognomonic for EoE and require histological confirmation.
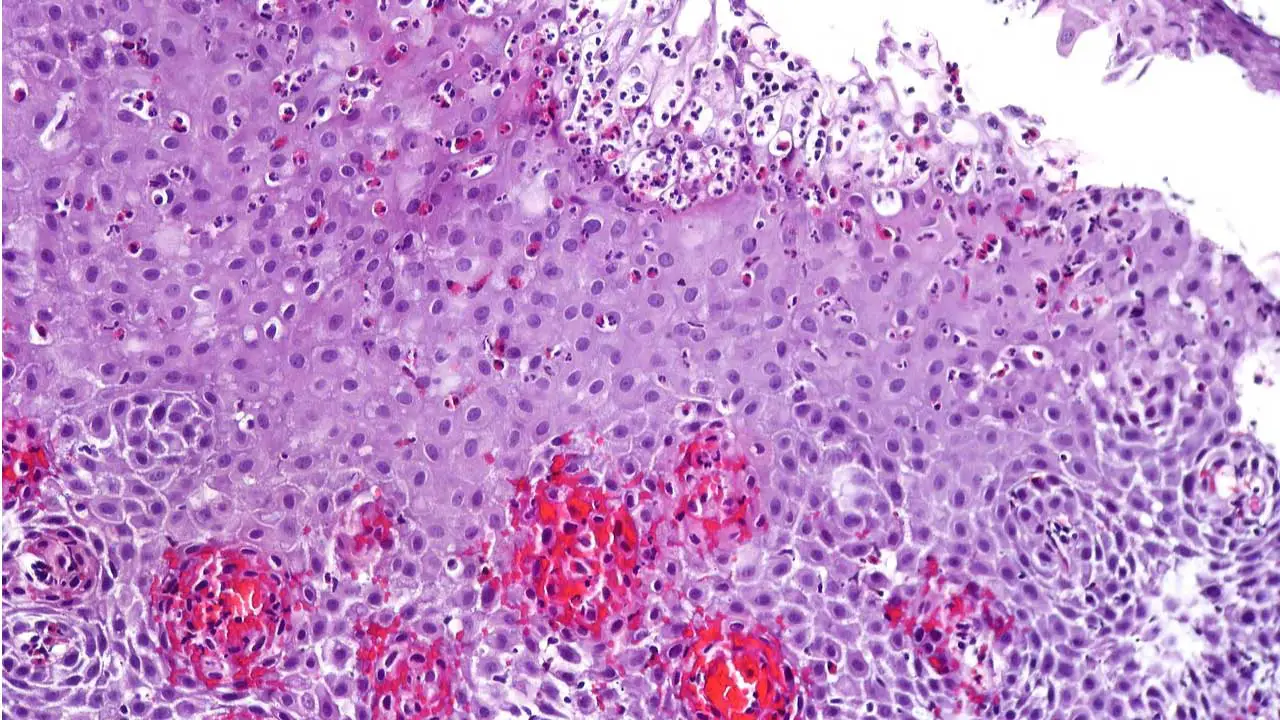
Histopathology
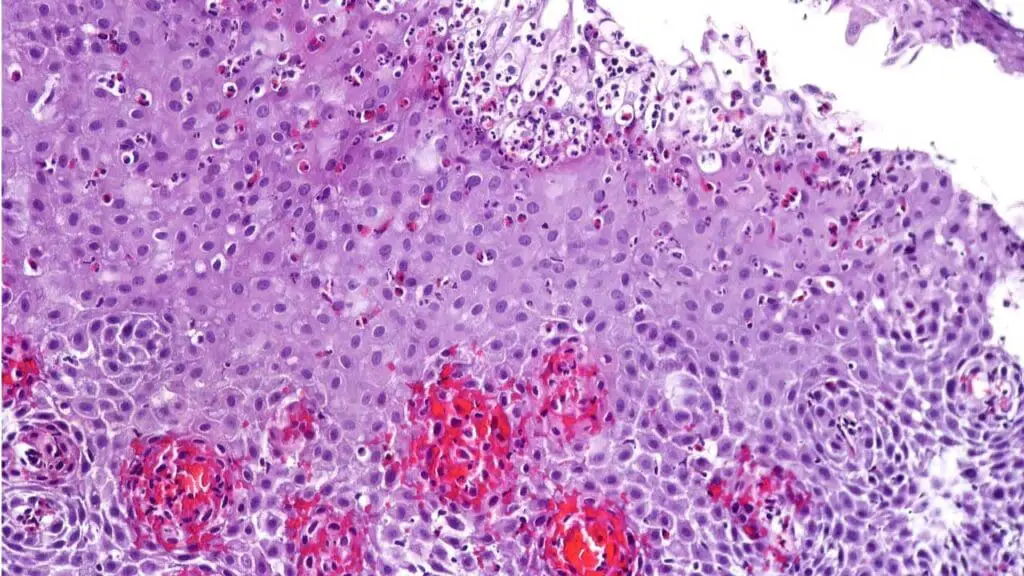
At least 6 biopsies from different locations within the esophagus are recommended. This is due to the patchy nature of eosinophilic infiltration. Taking biopsies from both the proximal and distal esophagus increases diagnostic yield.
The diagnostic hallmark of eosinophilic esophagitis (EoE) is the presence of ≥15 eosinophils per high-power field (HPF) in at least one biopsy specimen. This threshold distinguishes EoE from other conditions with mild esophageal eosinophilia.
Other Histological Features:
- Basal Cell Hyperplasia: Increased thickness of the basal layer of the esophageal epithelium.
- Surface Layering of Eosinophils: Eosinophils clustered along the epithelial surface.
- Dilated Intercellular Spaces (DIS): Widening of the spaces between epithelial cells, reflecting epithelial barrier dysfunction.
- Eosinophil microabscesses: Clumps of eosinophils within the epithelium.
- Fibrosis of the lamina propria.
Allergy Testing
These tests help identify potential food triggers.
- Skin Prick Tests: Detect immediate IgE-mediated allergies, but may not be as sensitive for delayed hypersensitivity reactions in EoE.
- Atopy Patch Tests: Assess delayed hypersensitivity reactions by applying allergen patches to the skin.
- Food Elimination Diets: Empiric or targeted elimination of common food allergens, followed by reintroduction to identify triggers.
- Component Resolved Diagnostics: This advanced form of allergy testing can help determine specific protein components of foods that a patient is reacting to.
Blood Tests
- Complete Blood Count (CBC) with Differential: May show mild eosinophilia in the peripheral blood, but this is not a consistent finding.
- IgE Levels: Total IgE levels may be elevated, especially in patients with atopic comorbidities, but are not specific for eosinophilic esophagitis (EoE).
Esophageal Manometry
This test is used to assess esophageal motility and identify any abnormalities. Findings may reveal impaired esophageal peristalsis or other motility disturbances in patients with eosinophilic esophagitis (EoE), especially those with strictures. This test is more useful in the differential diagnosis of other motility disorders such as achalasia.
pH Monitoring
pH monitoring helps to differentiate eosinophilic esophagitis (EoE) from GERD. A 24-hour pH monitoring assesses the amount of acid reflux in the esophagus. Although there can be an overlap of GERD and EoE, it is important to try and distinguish if the eosinophilia is caused by acid reflux. pH monitoring is useful to detect if a patient has abnormal acid reflux. It is also of value when evaluating PPI responsive esophageal eosinophilia.
Differential Diagnosis
When diagnosing Eosinophilic Esophagitis (EoE), it is crucial to consider and rule out several other conditions that can present with similar symptoms or endoscopic findings. This is essential to ensure the correct treatment plan is implemented, as therapies for other conditions may not be effective for Eosinophilic Esophagitis (EoE).
- Gastroesophageal Reflux Disease (GERD): This is perhaps the most common differential diagnosis. Patients with GERD also experience symptoms like heartburn and chest pain. However, unlike Eosinophilic Esophagitis (EoE), GERD is caused by acid reflux from the stomach, and its inflammation is not typically dominated by eosinophils to the same degree.A trial of a high-dose proton pump inhibitor (PPI) is often used to distinguish between the two, as some patients with esophageal eosinophilia may respond completely to PPIs (a condition known as PPI-responsive esophageal eosinophilia or PPI-REE).
- Crohn’s Disease of the Esophagus: This is a rare form of Crohn’s disease, an inflammatory bowel disease, that can affect the esophagus. It can also cause esophageal inflammation and symptoms. However, it is a separate disease process from Eosinophilic Esophagitis (EoE) and requires a different treatment approach.
- Infectious Esophagitis: Infections of the esophagus, caused by viruses (e.g., herpes simplex virus, cytomegalovirus) or fungi (e.g., Candida albicans), can lead to inflammation and symptoms of esophageal dysfunction. A biopsy is key to distinguishing these infections from Eosinophilic Esophagitis (EoE), as the histological findings will reveal the presence of infectious agents rather than a predominant eosinophilic infiltrate.
- Drug-induced Esophagitis: Certain medications, particularly bisphosphonates and some antibiotics, can cause inflammation and damage to the esophageal lining. A careful review of the patient’s medication history is important to rule out this cause. The symptoms typically resolve once the offending medication is stopped.
- Hypereosinophilic Syndrome (HES): This is a rare disorder characterized by a persistently high number of eosinophils in the blood and their infiltration into various organs, including the heart, lungs, and skin. While Eosinophilic Esophagitis (EoE) is considered a localized form of eosinophilic disease, HES is a systemic condition. Differentiating the two involves a comprehensive workup to look for eosinophilic infiltration in other organ systems.
| Condition | Key Clinical Features | Key Diagnostic Differences |
| GERD | Heartburn, chest pain | Eosinophils typically <15/HPF. Responds to PPIs. |
| Crohn’s Disease | Esophageal symptoms, plus GI tract inflammation (e.g., abdominal pain, diarrhea) | Biopsy shows granulomas and other Crohn’s-specific inflammation patterns. |
| Infectious Esophagitis | Odynophagia (painful swallowing), immunocompromised state | Biopsy reveals viral or fungal pathogens (e.g., herpes, Candida). |
| Drug-induced Esophagitis | Acute onset of odynophagia or dysphagia, history of taking specific medications (e.g., NSAIDs, bisphosphonates) | Symptoms resolve after discontinuing the medication. |
| Hypereosinophilic Syndrome | High peripheral eosinophil count, eosinophilic infiltration in multiple organs (e.g., heart, lungs) | Systemic disease, not limited to the esophagus. Diagnosis requires exclusion of other causes. |
Treatment and Management
The goals of eosinophilic esophagitis (EoE) treatment are to alleviate symptoms, improve esophageal function, and prevent complications such as strictures. Treatment strategies typically involve a combination of dietary, pharmacological, and endoscopic therapies.
A. Dietary Therapy
This is a cornerstone of EoE management, especially for identifying and eliminating food triggers. Dietary therapy requires close monitoring with repeat endoscopies to ensure efficacy.
- Elemental Diet: This involves consuming a formula containing amino acids, carbohydrates, and fats, completely eliminating intact proteins. Highly effective but can be challenging to adhere to long-term. Often used for initial induction of remission, especially in children.
- Empiric Elimination Diet (6-Food Elimination Diet): Involves eliminating the six most common food triggers: milk, wheat, soy, eggs, peanuts/tree nuts, and seafood. After a period of elimination, foods are reintroduced one at a time to identify triggers. It is a common first line approach.
- Targeted Elimination Diet: Based on allergy testing (skin prick tests, atopy patch tests, component resolved diagnostics). It eliminates only those foods identified as triggers. This can be more practical for long-term management.
B. Pharmacological Therapy
- Topical Corticosteroids: Fluticasone propionate and budesonide are commonly used. It is administered as swallowed aerosols or viscous slurries to coat the esophageal mucosa. It reduces eosinophilic inflammation and improves symptoms. Long-term use can have potential side effects, such as oral candidiasis.
- Proton Pump Inhibitors (PPIs): PPIs are often used as a first-line treatment, even before a definitive EoE diagnosis. While not directly targeting the allergic inflammation, they can reduce symptoms and, in some cases, resolve esophageal eosinophilia. PPI-responsive esophageal eosinophilia must be ruled out before the final diagnosis of EoE can be established.
- Biologics: Dupilumab is a monoclonal antibody that blocks IL-4 and IL-13 signaling. It has been shown to be effective in reducing eosinophilic inflammation and improving symptoms. It offers a systemic treatment option for patients who do not respond to topical corticosteroids or dietary therapy.
C. Endoscopic Dilation
It is used to treat esophageal strictures that cause dysphagia and food impaction. A balloon dilation or bougie dilation can widen the esophageal lumen. This carries a risk of esophageal perforation, so it should be performed by experienced endoscopists. It is not a treatment for the underlying disease process, but rather a treatment of a complication of the disease.
D. Long-Term Management and Monitoring
A regular follow-up with a gastroenterologist and allergist is essential. Follow-up endoscopies with biopsies are necessary to monitor disease activity and treatment response. Dietary maintenance is also crucial for preventing symptom recurrence. Constant monitoring for complications such as strictures and food impaction is vital and patient education is a large component of long term management.
Complications of Eosinophilic Esophagitis (EoE)
- Food Impaction: This is a common and distressing complication, especially in adults. Esophageal narrowing and strictures make it difficult for food to pass, leading to impaction. So this requires urgent endoscopic intervention to remove the impacted food. Recurrent food impactions can significantly impact quality of life.
- Esophageal Strictures and Narrowing:nChronic inflammation leads to fibrosis and remodeling of the esophageal wall. This results in the formation of strictures, which progressively narrow the esophageal lumen. Strictures contribute to dysphagia and increase the risk of food impaction. Long term unchecked inflammation almost always leads to some form of esophageal remodeling.
- Esophageal Perforation (Rare): While rare, esophageal perforation can occur during endoscopic procedures, particularly dilation. It is a serious complication that requires immediate medical attention. Also, in rare cases, a food impaction can lead to perforation.
- Impact on Quality of Life: EoE can significantly affect patients’ quality of life due to dysphagia, food avoidance, and anxiety related to eating. Children may experience social isolation and nutritional deficiencies. While adults may struggle with work productivity and social activities. The constant need for dietary restrictions can cause increased anxiety.
Prognosis
EoE is a chronic disease that typically requires long-term management. While symptoms can be effectively controlled with treatment, relapse is common if treatment is discontinued. Most patients respond well to dietary therapy, topical corticosteroids, or biologics. Early diagnosis and intervention can prevent or minimize complications such as strictures. Adherence to treatment is crucial for long-term symptom control.
With appropriate management, most patients can lead relatively normal lives. Regular monitoring and follow-up are essential to detect and treat complications.
Early diagnosis and treatment can prevent long term complications such as stricture formation. Early treatment can also prevent the development of compensatory eating behaviors in children.
While not always a cure, long term remission is a realistic goal for many patients. Remission can be histological, symptomatic, or both. Maintaining remission often requires continued dietary or pharmacological therapy.
Frequently Asked Questions (FAQs)
Is eosinophilic esophagitis serious?
Yes, Eosinophilic Esophagitis is considered a serious, chronic condition. While it is not typically life-threatening, it can significantly impact a person’s quality of life and, if left untreated, can lead to severe complications.
What are the triggers for eosinophilic oesophagitis?
The triggers for eosinophilic esophagitis (EoE) are primarily an allergic response to certain substances.
- Food Allergens: Eosinophilic esophagitis (EoE) is considered an allergen-driven immune response, and food proteins are the most common triggers. These can be IgE-mediated or non-IgE-mediated food allergies.
- Aeroallergens: Environmental triggers, such as aeroallergens (e.g., pollen), also play a role in the “two-hit hypothesis” for the disease.
Can eosinophilic esophagitis start suddenly?
Eosinophilic esophagitis (EoE) is a chronic, immune-mediated disease. This suggests that the underlying inflammation and damage to the esophagus typically develop over time rather than starting suddenly.
However, a common symptom in adolescents and adults is food impaction, which is a sudden and acute event where food gets stuck in the narrowed esophagus. This sudden, alarming event is often what leads to the diagnosis of the underlying, chronic condition.
Can EoE affect bowels?
EoE is a type of Eosinophilic Gastrointestinal Disease (EGID). While EoE is specific to the esophagus, other EGIDs can affect different parts of the digestive tract, including the stomach, small intestine, and large intestine (bowels).\
How to calm an EoE flare up?
Topical steroids, such as swallowed fluticasone or budesonide, are a key treatment. These medications directly target the esophageal lining to reduce the eosinophilic infiltration and inflammation that cause the symptoms of a flare-up.
Do people with EoE cough a lot?
Coughing is not considered a primary or typical symptom of Eosinophilic Esophagitis (EoE), but it can occur.
A chronic cough is sometimes an early sign of EoE, particularly in children. The cough may be a result of the same allergic inflammation that causes EoE, or it could be due to coexisting conditions that are often seen with EoE, such as asthma or gastroesophageal reflux disease (GERD). In these cases, treating the underlying EoE is the key to managing the cough.
Do antihistamines help with EoE?
Antihistamines are not considered a primary or effective treatment for Eosinophilic Esophagitis (EoE).
EoE is an immune-mediated disease driven by an inflammatory response involving eosinophils and specific cytokines like IL-5 and IL-13, not the histamine-mediated pathway that antihistamines target.
While some clinical trials have explored the use of antihistamines, standard medical guidelines and the treatment protocols focus on dietary therapy, proton pump inhibitors (PPIs), and topical steroids. Therefore, an individual with EoE would typically rely on these proven therapies rather than antihistamines to manage their condition.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Lehman HK, Lam W. Eosinophilic Esophagitis. Immunol Allergy Clin North Am. 2021 Nov;41(4):587-598. doi: 10.1016/j.iac.2021.07.011. PMID: 34602230.
- Patel RV, Hirano I, Gonsalves N. Eosinophilic Esophagitis: Etiology and Therapy. Annu Rev Med. 2021 Jan 27;72:183-197. doi: 10.1146/annurev-med-052819-023848. Epub 2020 Nov 23. PMID: 33228437.
- Gonsalves NP, Aceves SS. Diagnosis and treatment of eosinophilic esophagitis. J Allergy Clin Immunol. 2020 Jan;145(1):1-7. doi: 10.1016/j.jaci.2019.11.011. PMID: 31910983; PMCID: PMC6986782.
- Lucendo A, Groetch M, Gonsalves N. Dietary Management of Eosinophilic Esophagitis. Immunol Allergy Clin North Am. 2024 May;44(2):223-244. doi: 10.1016/j.iac.2023.12.009. Epub 2024 Feb 16. PMID: 38575220.
- Barni S, Arasi S, Mastrorilli C, Pecoraro L, Giovannini M, Mori F, Liotti L, Saretta F, Castagnoli R, Caminiti L, Cianferoni A, Novembre E. Pediatric eosinophilic esophagitis: a review for the clinician. Ital J Pediatr. 2021 Nov 22;47(1):230. doi: 10.1186/s13052-021-01178-2. PMID: 34809686; PMCID: PMC8609874.
- Uchida AM, Burk CM, Rothenberg ME, Furuta GT, Spergel JM. Recent Advances in the Treatment of Eosinophilic Esophagitis. J Allergy Clin Immunol Pract. 2023 Sep;11(9):2654-2663. doi: 10.1016/j.jaip.2023.06.035. Epub 2023 Jun 28. PMID: 37391018; PMCID: PMC10530275.