TL;DR
Erythropoietin (EPO) is a vital hormone primarily produced by the kidneys. It plays a crucial role in stimulating the production of red blood cells in the bone marrow, a process known as erythropoiesis.
Key Functions of EPO ▾
- Stimulates Red Blood Cell Production: EPO triggers the bone marrow to produce more red blood cells, increasing the blood’s oxygen-carrying capacity.
- Regulates Hemoglobin Synthesis: EPO helps regulate the production of hemoglobin, the iron-containing protein in red blood cells that binds to oxygen.
- Influences Iron Metabolism: EPO indirectly affects iron metabolism by regulating hepcidin, a hormone that controls iron absorption and release.
Causes of High EPO Levels ▾
- Physiological Causes: High altitude, anemia
- Pathological Causes: Renal cell carcinoma, hepatocellular carcinoma
Causes of Low EPO Levels ▾
- Chronic Kidney Disease: As kidney function declines, EPO production decreases.
- Certain Anemias: Pure red cell aplasia
Clinical Uses of EPO ▾
- Treatment of Anemia: EPO is used to treat anemia associated with chronic kidney disease, cancer chemotherapy, and other conditions.
- Potentiating Autologous Blood Transfusion: EPO can help patients donate more blood pre-operatively, reducing the need for allogeneic transfusions.
Potential Side Effects ▾
- Hypertension
- Thromboembolic events
- Pure red cell aplasia
Monitoring and Management
- Regular monitoring of blood counts, blood pressure, and kidney function is essential.
- Dosage adjustments may be necessary to optimize therapy and minimize side effects.
*Click ▾ for more information
Introduction
Erythropoietin (EPO) is a vital hormone primarily produced by the kidneys in response to cellular hypoxia, or low oxygen levels.
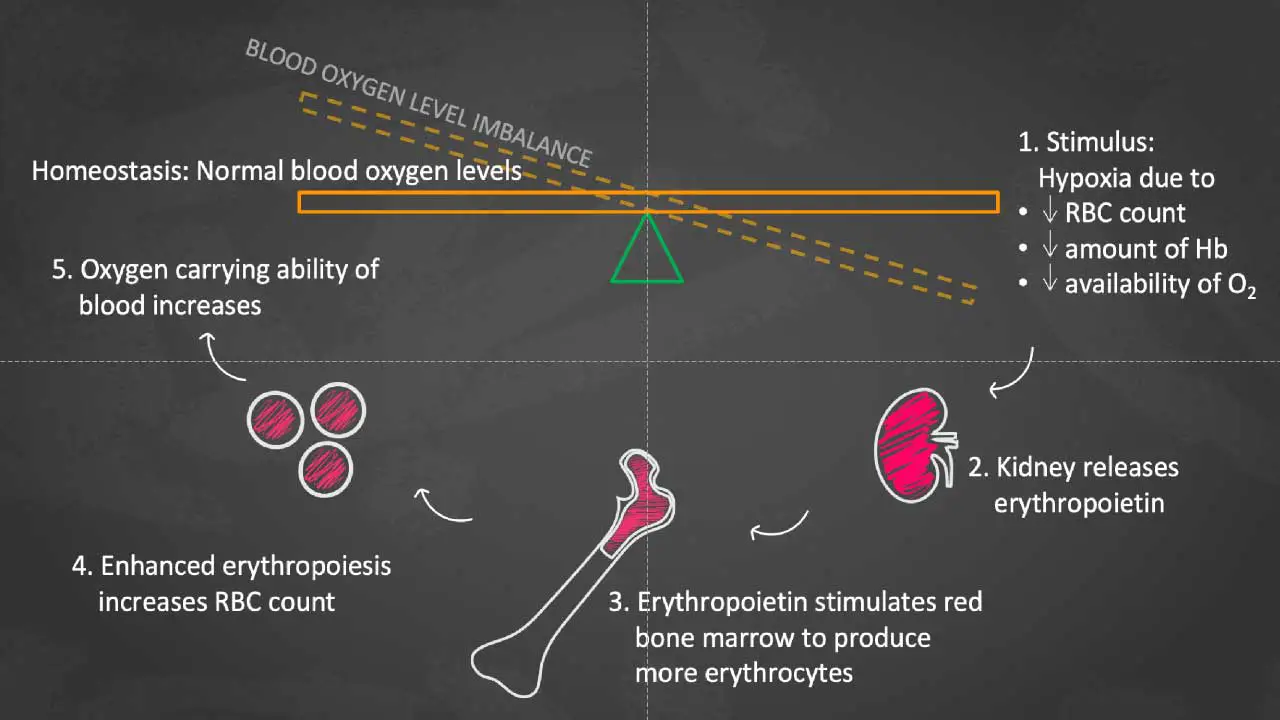
It plays a crucial role in regulating red blood cell production, or erythropoiesis, in the bone marrow. When oxygen levels decline, the kidneys release EPO, which stimulates the bone marrow to increase the production of red blood cells. These red blood cells then carry oxygen throughout the body, helping to restore normal oxygen levels.
A Brief Historical Overview of EPO Discovery and Research
The discovery of erythropoietin is a fascinating story that dates back to the early 20th century. Here’s a brief historical overview:
- Early 1900s: Scientists first observed that blood loss stimulated the production of red blood cells. However, the exact mechanism behind this process remained unknown.
- 1950s: Researchers began to isolate and purify a substance from the kidneys that could stimulate red blood cell production. This substance was later named erythropoietin.
- 1980s: The gene encoding EPO was cloned, allowing for the production of recombinant human erythropoietin (rHuEPO). This breakthrough led to the development of synthetic EPO, which revolutionized the treatment of anemia associated with chronic kidney disease and cancer chemotherapy.
- 1990s: The widespread use of rHuEPO also raised concerns about its potential misuse in sports to enhance athletic performance. This led to the development of sophisticated tests to detect the use of EPO in athletes.
Today, EPO remains a critical therapeutic agent for treating various forms of anemia. Ongoing research continues to explore its potential in other medical conditions and to develop novel EPO-based therapies.
Function of Erythropoietin
Primary Role in Erythropoiesis
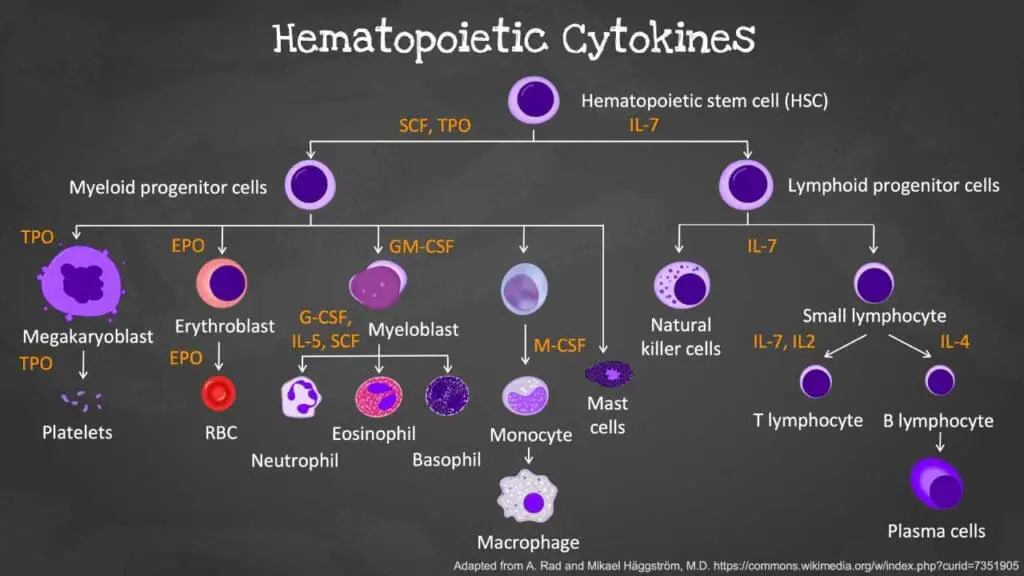
- Stimulation of Red Blood Cell Production: Erythropoietin (EPO) primarily targets the bone marrow, where it stimulates the proliferation and differentiation of hematopoietic stem cells into red blood cell precursors. This process, known as erythropoiesis, leads to an increase in the production of red blood cells.
- Promotion of Red Blood Cell Maturation: Erythropoietin (EPO) not only stimulates the production of red blood cells but also promotes their maturation. It helps in the synthesis of hemoglobin, the oxygen-carrying protein within red blood cells.
Regulation of Hemoglobin Synthesis
- Hemoglobin Induction: Erythropoietin (EPO) induces the transcription of genes involved in hemoglobin synthesis, including genes for globin chains (alpha and beta) and heme.
Regulation of Iron Metabolism
While EPO’s primary function is to stimulate red blood cell production, it indirectly influences iron metabolism.
- Hepcidin Regulation: Erythropoietin (EPO)-stimulated erythropoiesis leads to the production of a hormone called erythroferrone. Erythroferrone suppresses the production of hepcidin, a hormone that regulates iron absorption from the gut and its release from stores. By suppressing hepcidin, erythropoietin (EPO) indirectly increases iron availability for red blood cell production.
- Iron Absorption and Utilization: Increased iron absorption from the diet is essential to meet the demands of increased erythropoiesis. Erythropoietin (EPO) indirectly promotes iron absorption by downregulating hepcidin. Additionally, erythropoietin (EPO) stimulates the release of iron from storage sites, such as the liver and spleen, making it available for red blood cell production.
By regulating these processes, erythropoietin (EPO) ensures that the body maintains adequate oxygen-carrying capacity, which is essential for various physiological functions, including energy production, tissue repair, and organ function.
Production of Erythropoietin
Primary Site of Production: Kidneys
The kidneys are the primary site of erythropoietin (EPO) production. Specialized cells within the kidney, primarily in the peritubular cells of the cortex, sense changes in oxygen levels in the blood. When oxygen levels decrease, these cells respond by synthesizing and releasing EPO into the bloodstream.
Secondary Site: Liver
While the kidneys are the major source of erythropoietin (EPO), the liver can also produce erythropoietin (EPO), particularly during fetal development and in certain pathological conditions, such as liver disease. However, the liver’s contribution to overall EPO production is relatively minor compared to the kidneys.
Hormonal Regulation of Erythropoietin (EPO) Production
The production of erythropoietin (EPO) is primarily regulated by a negative feedback loop involving oxygen levels in the blood. When oxygen levels decrease, the kidneys sense this change and increase erythropoietin (EPO) production. As erythropoietin (EPO) stimulates red blood cell production, oxygen levels in the blood increase, which in turn decreases erythropoietin (EPO) production.
Factors Influencing Erythropoietin (EPO) Levels
Several factors can influence erythropoietin (EPO) levels:
- Hypoxia: Low oxygen levels in the blood are the primary stimulus for erythropoietin (EPO) production. Conditions such as high altitude, anemia, and lung disease can lead to increased erythropoietin (EPO) levels.
- Anemia: When the number of red blood cells or the amount of hemoglobin decreases, the body’s oxygen-carrying capacity is reduced, leading to hypoxia and increased erythropoietin (EPO) production.
- Kidney Disease: Kidney disease can impair the kidney’s ability to produce erythropoietin (EPO), leading to anemia.
- Androgens: Androgens, such as testosterone, can stimulate erythropoietin (EPO) production.
- Other Factors: Certain medications, such as corticosteroids and anti-inflammatory drugs, can also influence erythropoietin (EPO) production.
Laboratory Tests for Erythropoietin
Immunoassay is a biochemical technique that utilizes antibodies to detect specific substances, such as hormones like EPO. In the case of EPO measurement, antibodies specific to EPO are used to bind to the hormone in the serum sample. This binding can be detected using various methods, such as:
- Enzyme-linked immunosorbent assay (ELISA): This method involves using enzymes linked to antibodies to produce a color change, which can be measured to quantify the amount of EPO present.
- Chemiluminescent immunoassay: This technique uses luminescent chemicals to produce light, which is measured to detect the amount of EPO.
Erythropoietin Levels
Normal Reference Ranges
The normal reference range for erythropoietin (EPO) levels can vary slightly between laboratories. However, generally, normal erythropoietin (EPO) levels are:
- Adults: 4-24 mU/mL
- Children: 2-20 mU/mL
It’s important to note that these are general ranges, and individual values may vary.
Elevated Erythropoietin (EPO) Levels
Physiological Causes
- High Altitude: Living at high altitudes can lead to decreased oxygen levels in the blood, stimulating the kidneys to produce more EPO.
- Anemia: Conditions that cause anemia, such as iron deficiency or vitamin B12 deficiency, can increase erythropoietin (EPO) levels as the body tries to compensate for the low red blood cell count.
Pathological Causes
- Renal Failure: Kidney disease can impair the kidney’s ability to produce erythropoietin (EPO), leading to low levels. However, in some cases, especially early in the course of kidney disease, erythropoietin (EPO) levels may be elevated as the kidneys attempt to compensate for the reduced kidney function.
- Tumors: Certain tumors, particularly those of the kidney, liver, and brain, can produce erythropoietin (EPO)-like substances, leading to elevated erythropoietin (EPO) levels and secondary erythrocytosis (increased red blood cell count).
Decreased Erythropoietin (EPO) Levels
Decreased erythropoietin (EPO) levels are relatively rare but can occur in conditions such as:
- Certain Anemias: In some types of anemia, such as pure red cell aplasia, the bone marrow fails to produce red blood cells, even in the presence of adequate erythropoietin (EPO).
- Kidney Failure: As kidney disease progresses, erythropoietin (EPO) production declines, leading to anemia.
Clinical Uses of Erythropoietin
Erythropoietin (EPO) is a valuable therapeutic agent used to treat various conditions characterized by anemia, or a deficiency of red blood cells. Recombinant EPO is a synthetic form of erythropoietin (EPO) produced through biotechnology. It is widely used in clinical practice due to its effectiveness and safety profile.
Treatment of Anemia
- Chronic Kidney Disease (CKD): Kidney disease can impair the kidney’s ability to produce EPO, leading to anemia. Recombinant human erythropoietin (rHuEPO) is used to stimulate red blood cell production and alleviate anemia in CKD patients.
- Cancer Chemotherapy-Induced Anemia: Chemotherapy can damage bone marrow cells, leading to a decrease in red blood cell production and anemia. rHuEPO can be used to help stimulate red blood cell production and reduce the need for blood transfusions in cancer patients undergoing chemotherapy.
- Anemia of Chronic Disease: Chronic inflammatory diseases, such as rheumatoid arthritis and inflammatory bowel disease, can cause anemia of chronic disease. rHuEPO can be used to treat anemia in these patients, although its effectiveness may vary.
Other Potential Uses
- Potentiate Autologous Blood Transfusion: Autologous blood donation, where a patient’s own blood is collected pre-surgery and re-transfused, minimizes risks of bloodborne infections and transfusion reactions. EPO can enhance this process by stimulating red blood cell production, enabling patients, especially those with low hemoglobin or anemia, to donate more blood preoperatively.
- Regenerative Medicine: EPO has been studied for its potential role in tissue repair and regeneration, particularly in the context of wound healing and neurological disorders.
- Sports Performance Enhancement: While the use of EPO for athletic performance enhancement is banned, it has been used illegally by some athletes to increase red blood cell count and improve oxygen delivery to muscles.
Potential Side Effects and Complications of Erythropoietin Therapy
While EPO is a valuable therapeutic agent, it can have potential side effects and complications, particularly if used inappropriately or in high doses. Some of the most common side effects include:
- Hypertension: EPO can increase blood pressure, especially in patients with underlying cardiovascular disease.
- Thromboembolic Events: EPO therapy can increase the risk of blood clots, such as deep vein thrombosis and pulmonary embolism, particularly in patients with risk factors for thrombosis.
- Pure Red Cell Aplasia (PRCA): A rare but serious side effect, PRCA is characterized by a severe decrease in red blood cell production. It can be caused by the development of antibodies against EPO or its receptor.
Other potential side effects include:
- Headache
- Fatigue
- Flu-like symptoms
- Bone pain
To minimize the risk of side effects, it is important to monitor patients closely during erythropoietin (EPO) therapy. This includes regular blood tests to check hemoglobin levels, blood pressure, and kidney function. In some cases, adjusting the dosage of erythropoietin (EPO) or using other medications may be necessary to manage side effects.
Disclaimer: This article is intended for informational purposes only and is specifically targeted towards medical students. It is not intended to be a substitute for informed professional medical advice, diagnosis, or treatment. While the information presented here is derived from credible medical sources and is believed to be accurate and up-to-date, it is not guaranteed to be complete or error-free. See additional information.
References
- Shahab MH, Saifullah Khan S. Erythropoietin Administration for Anemia Due to Chronic Kidney Disease – Subcutaneous OR Intravenous, What Do We Know So Far? Cureus. 2020 Sep 10;12(9):e10358. doi: 10.7759/cureus.10358. PMID: 33062481; PMCID: PMC7549864.
- Macdougall IC. Treatment of renal anemia with recombinant human erythropoietin. Curr Opin Nephrol Hypertens. 1992 Dec;1(2):210-9. doi: 10.1097/00041552-199212000-00005. PMID: 1345620.
- Shermock KM, Horn E, Rice TL. Erythropoietic agents for anemia of critical illness. Am J Health Syst Pharm. 2008 Mar 15;65(6):540-6. doi: 10.2146/ajhp070225. PMID: 18319499.



